Introduction
Introduction
Dr. Sarah Faubel created this 2-hour lecture block. The idea was to look at 4 different theater of operations and do a deep dive on how the causes and treatments of acute kidney injury differ. This is a salute to Bayesian logic and attempts to give doctors a refined view of pre-test probabilities for the etiologies of AKI depending on the clinical scenario. Great idea.
The lecture session is divided into four talks by four different speakers
- AKI in the Neuro ICU
- AKI in the Trauma Ward
- AKI in the Cancer Ward
- AKI in the BMT ward
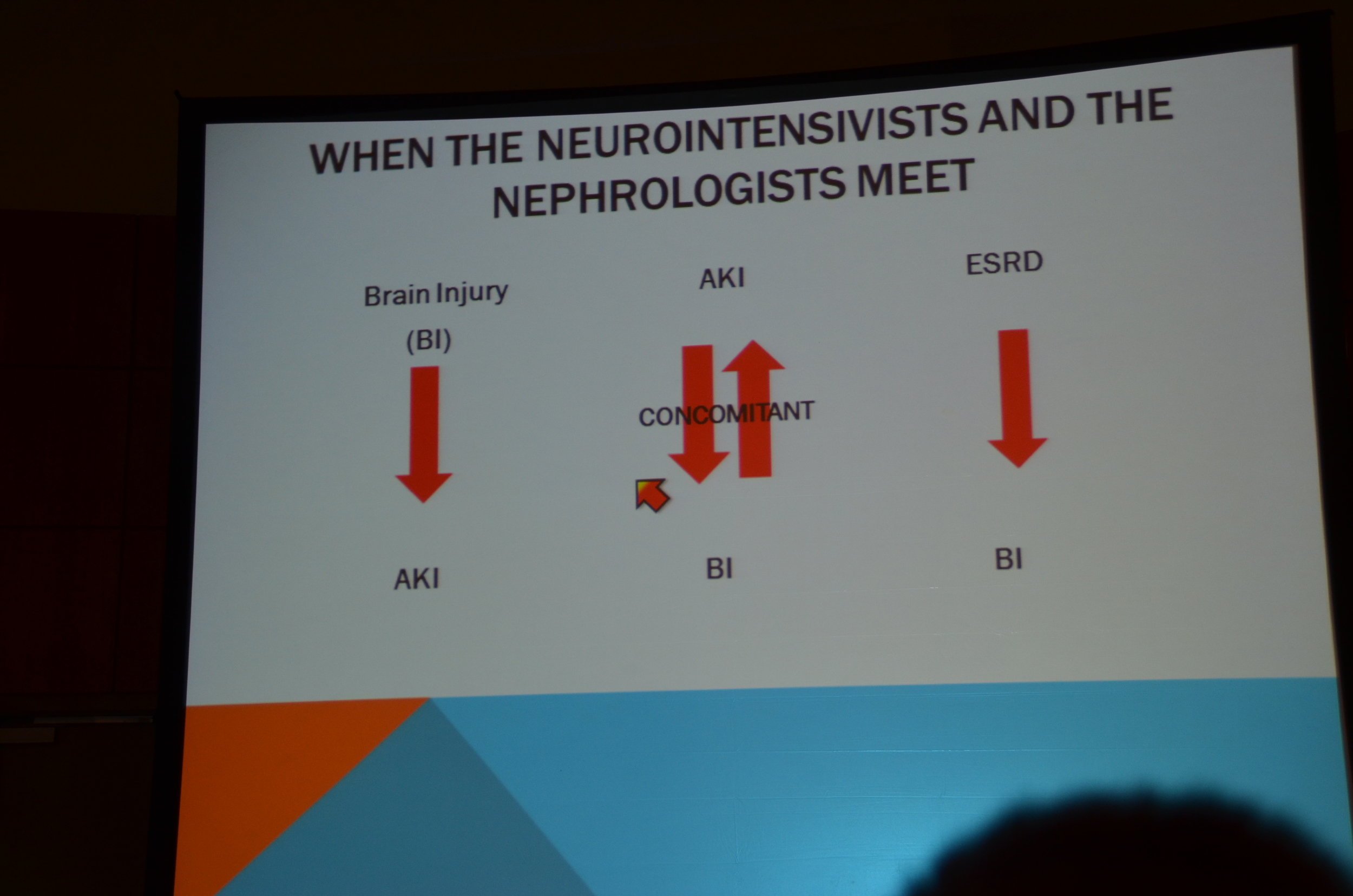
Neuro ICU
Neuro ICU
First up is Thomas Berl of University of Colorado



My post for eAJKD
Kidney Week 2012: Acute Kidney Injury in the Neuro ICU
One of the talks was Dr. Berl on AKI in the neurological unit.
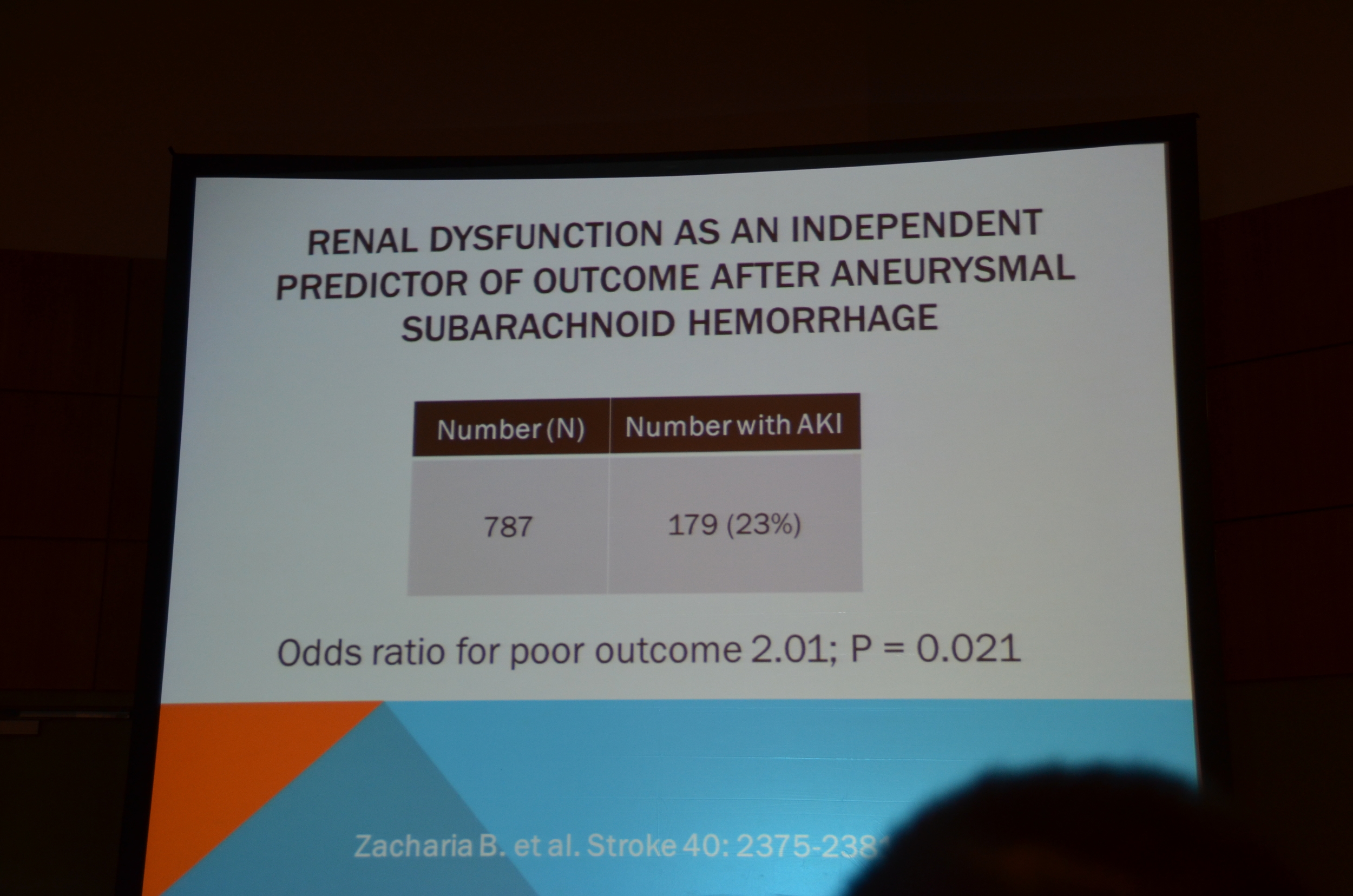
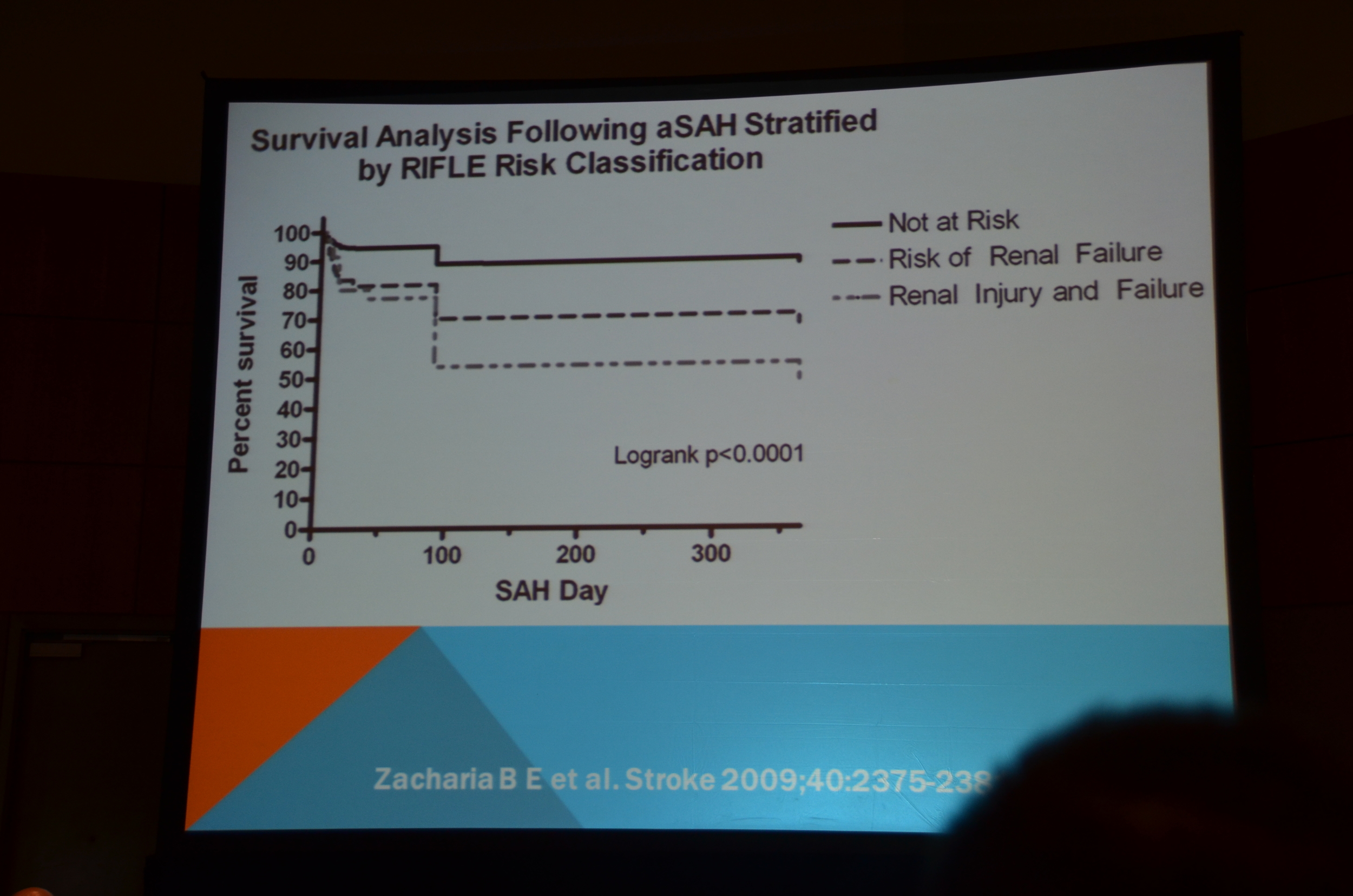
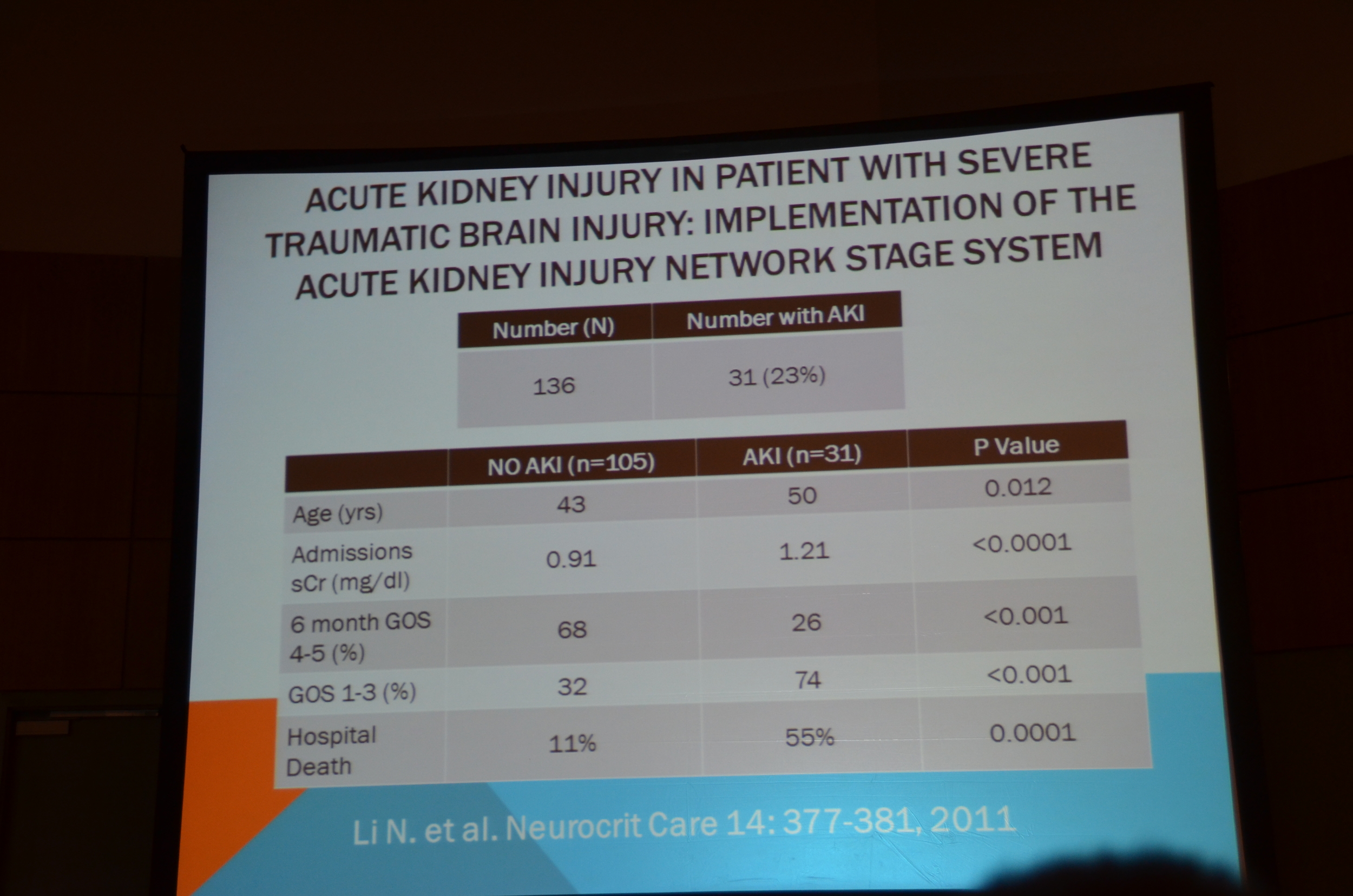
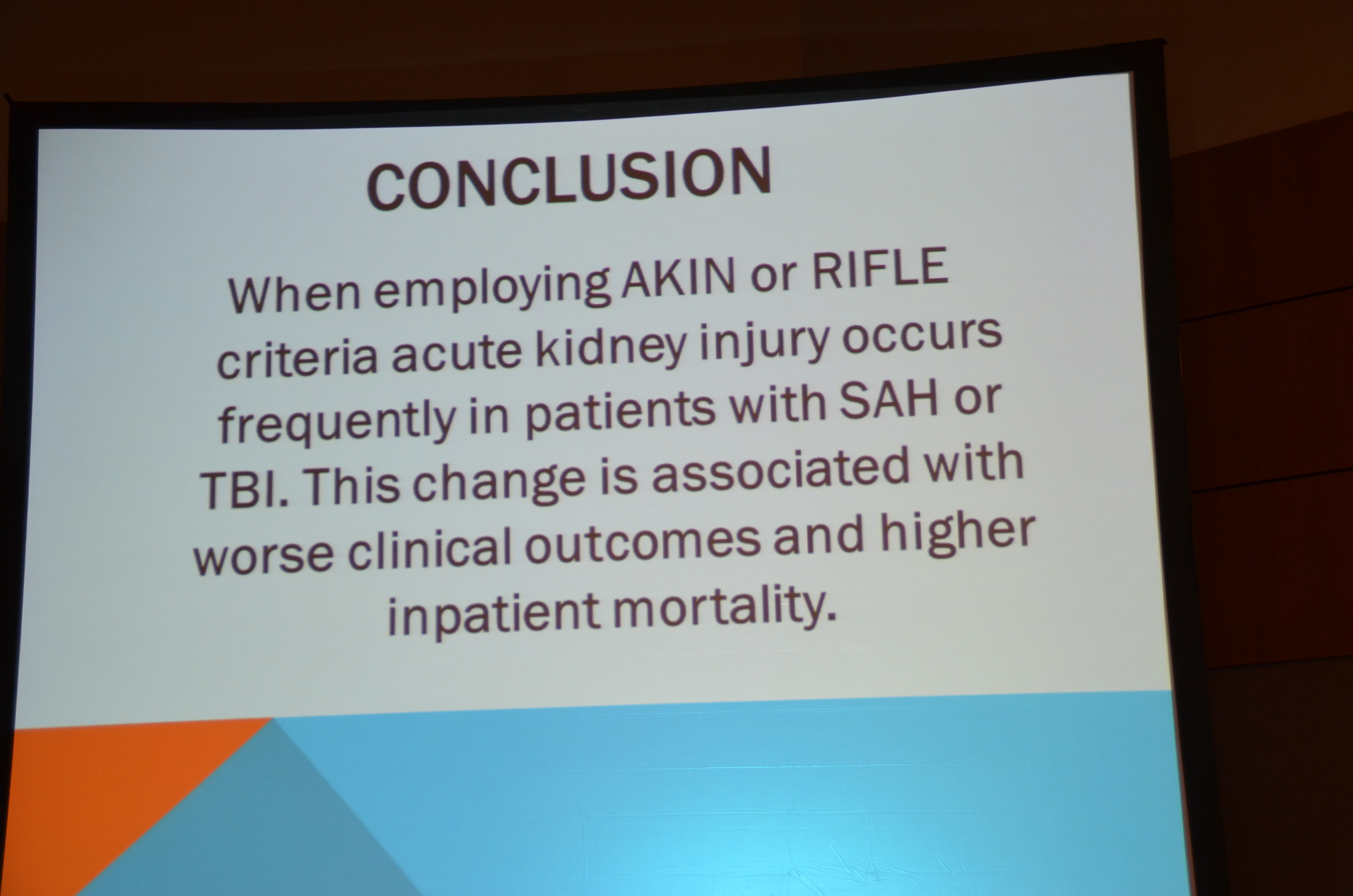
The incidence of AKI, using RIFLE criteria, was 23% following a subarachnoid hemorrhage. Importantly he found that the severity of AKI predicted survival with the poorest outcomes associated with RIFLE stage: Failure.
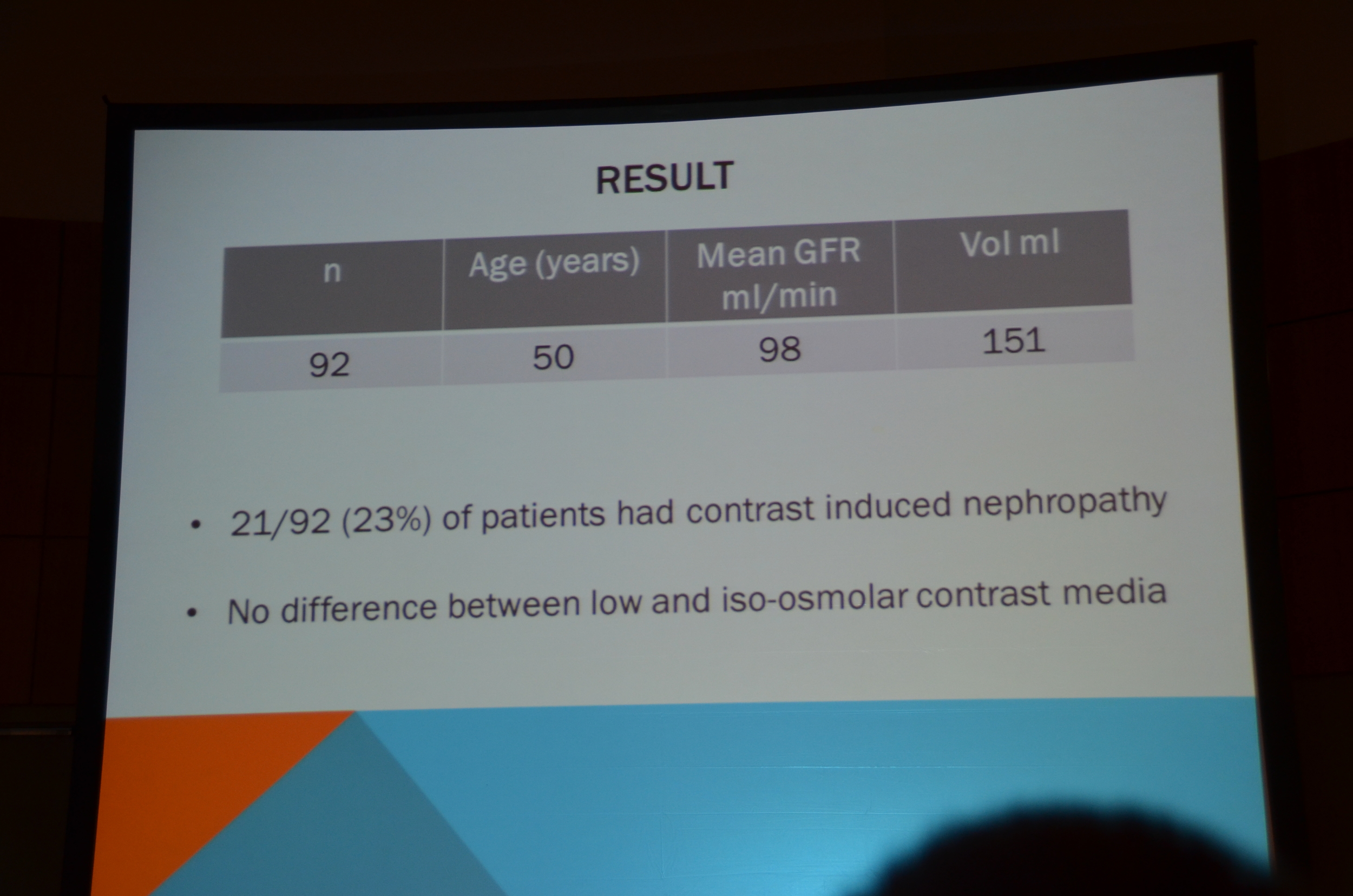
He then discussed contrast nephropathy. Serafin et al found a very high incidence of contrast nephropathy following intra-arteriole administration of contrast. Contrast nephropathy occurred in 23% of patients, despite a pre-morbid average GFR of 98 mL/min. They did not see any difference between low and iso-osmolar contrast.
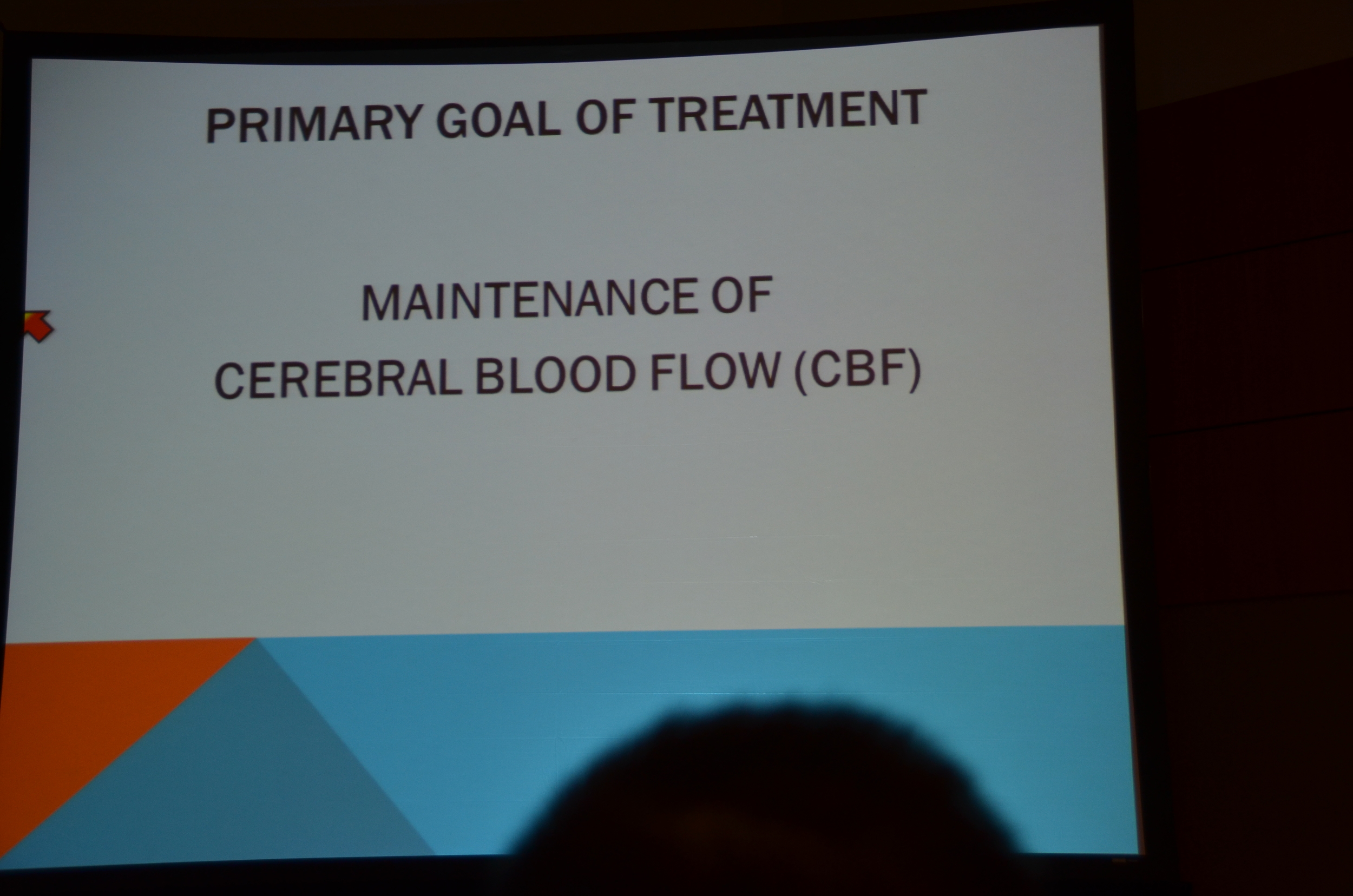
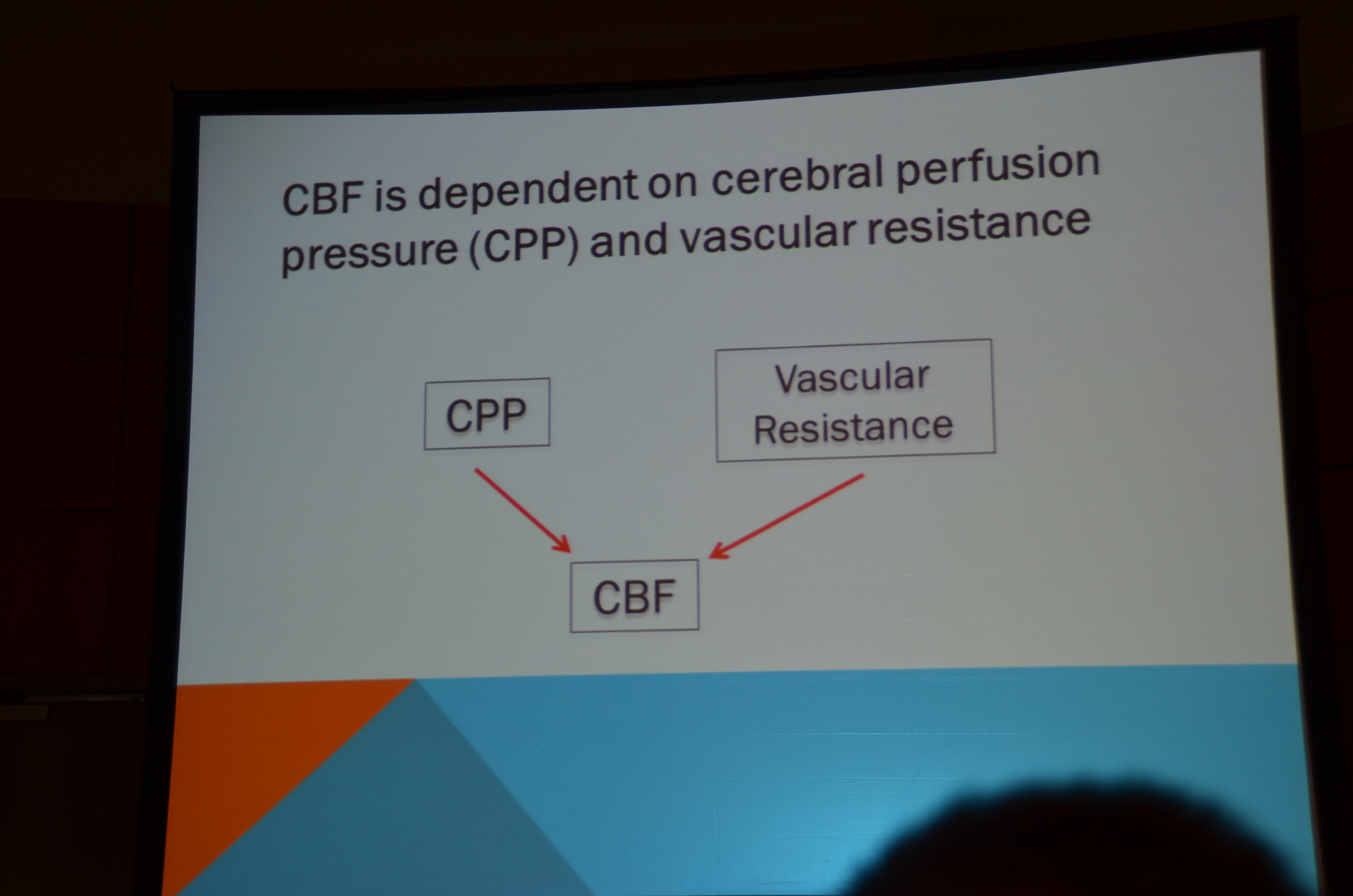
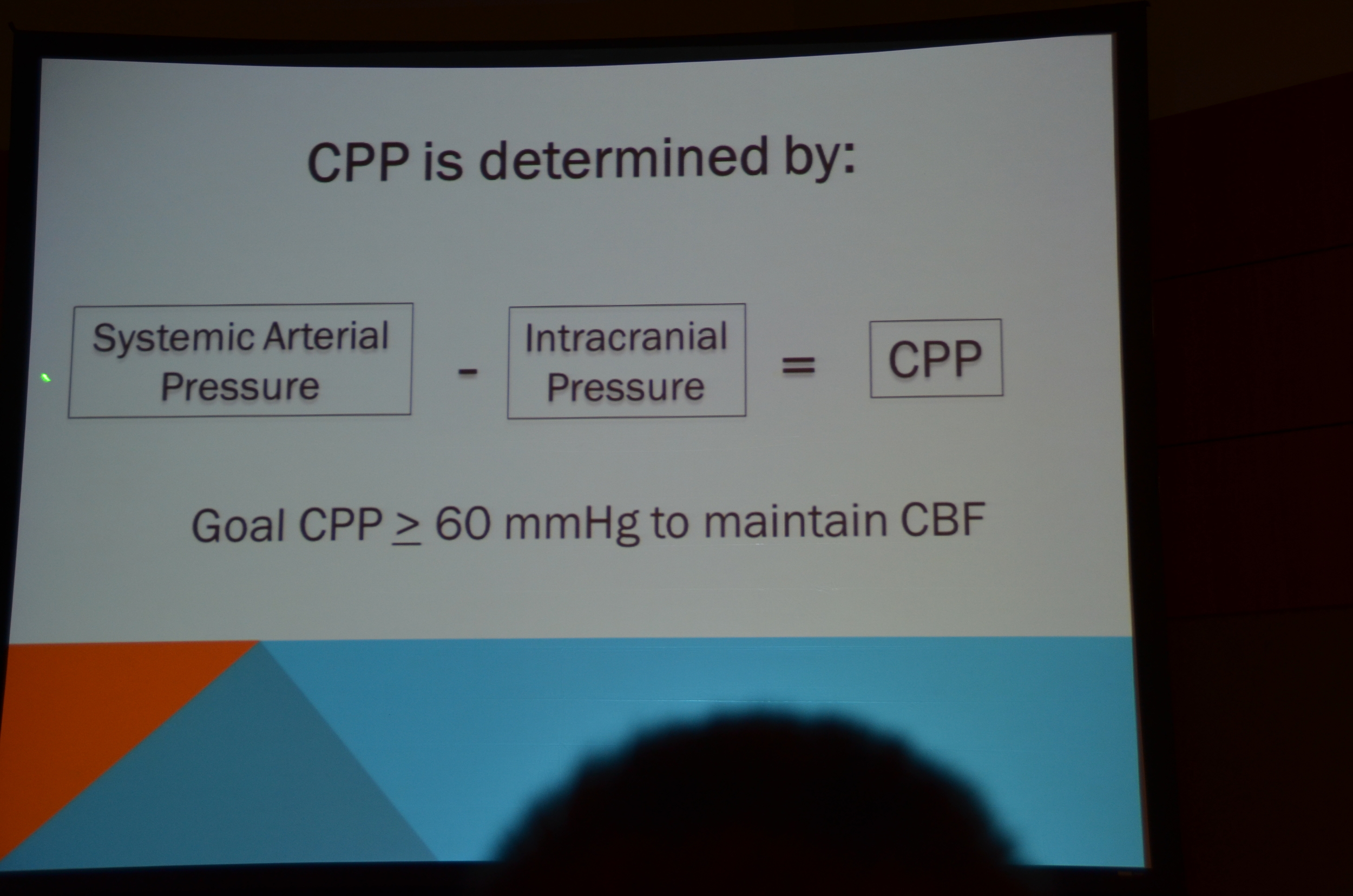
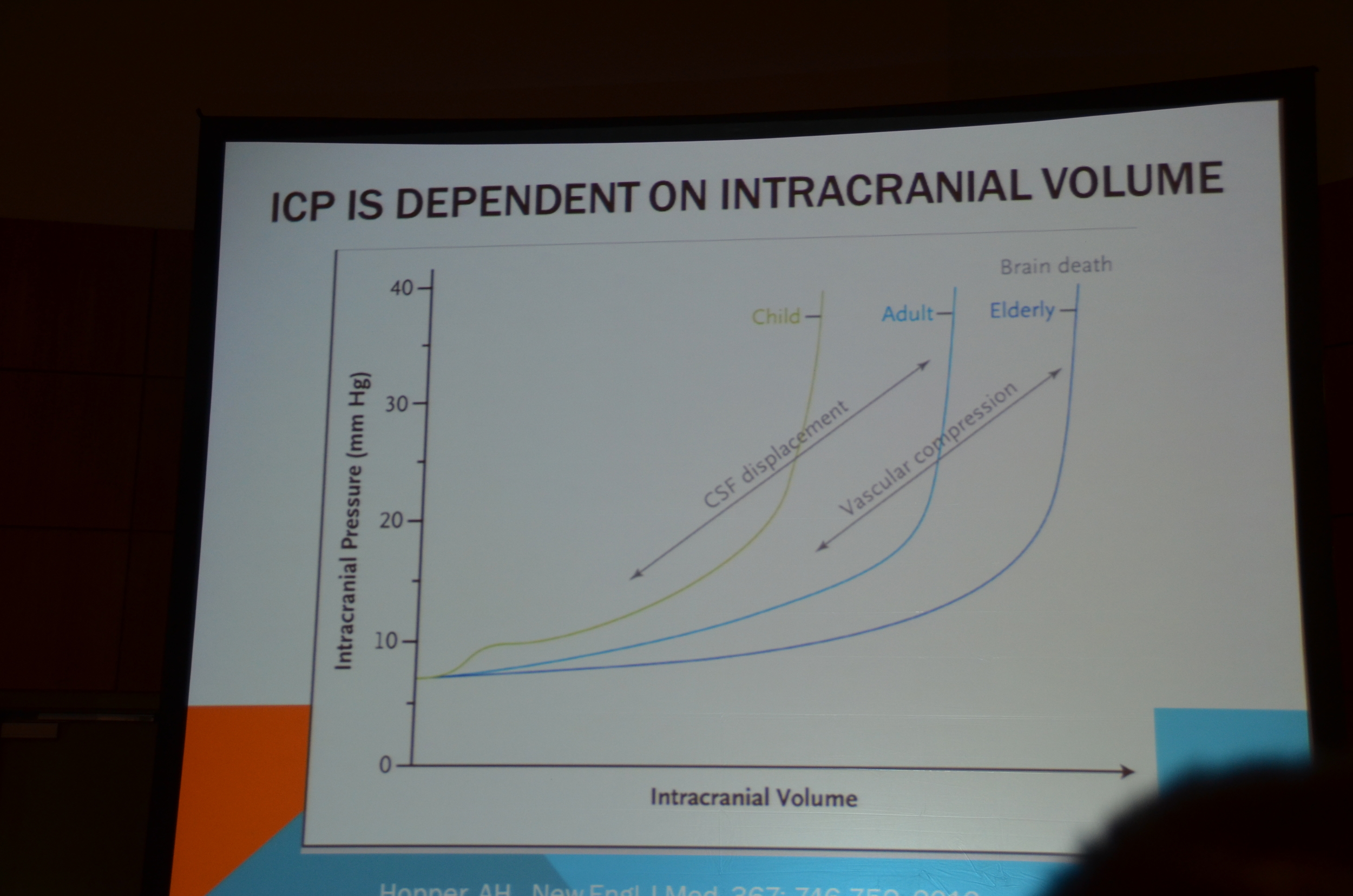
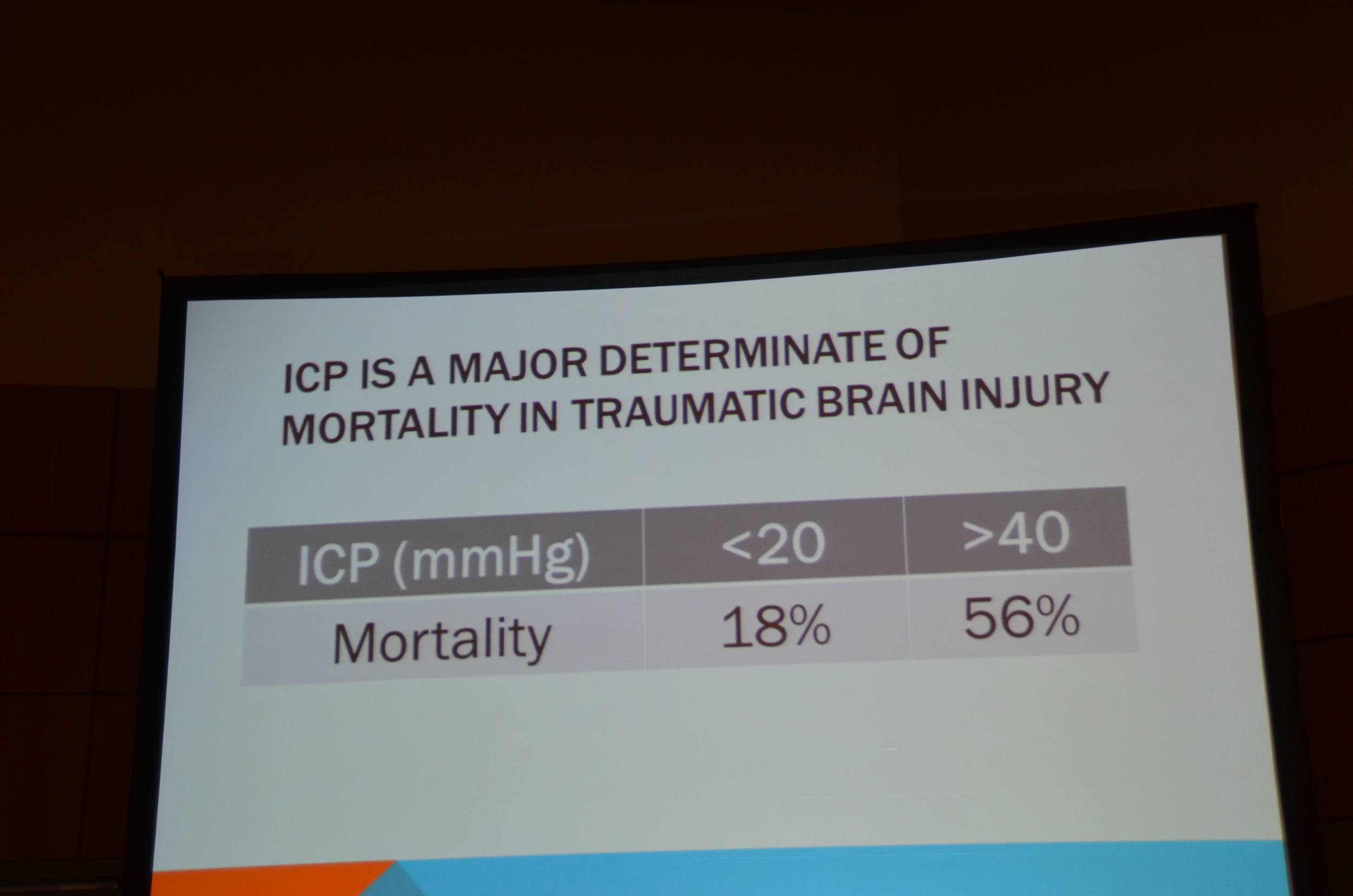
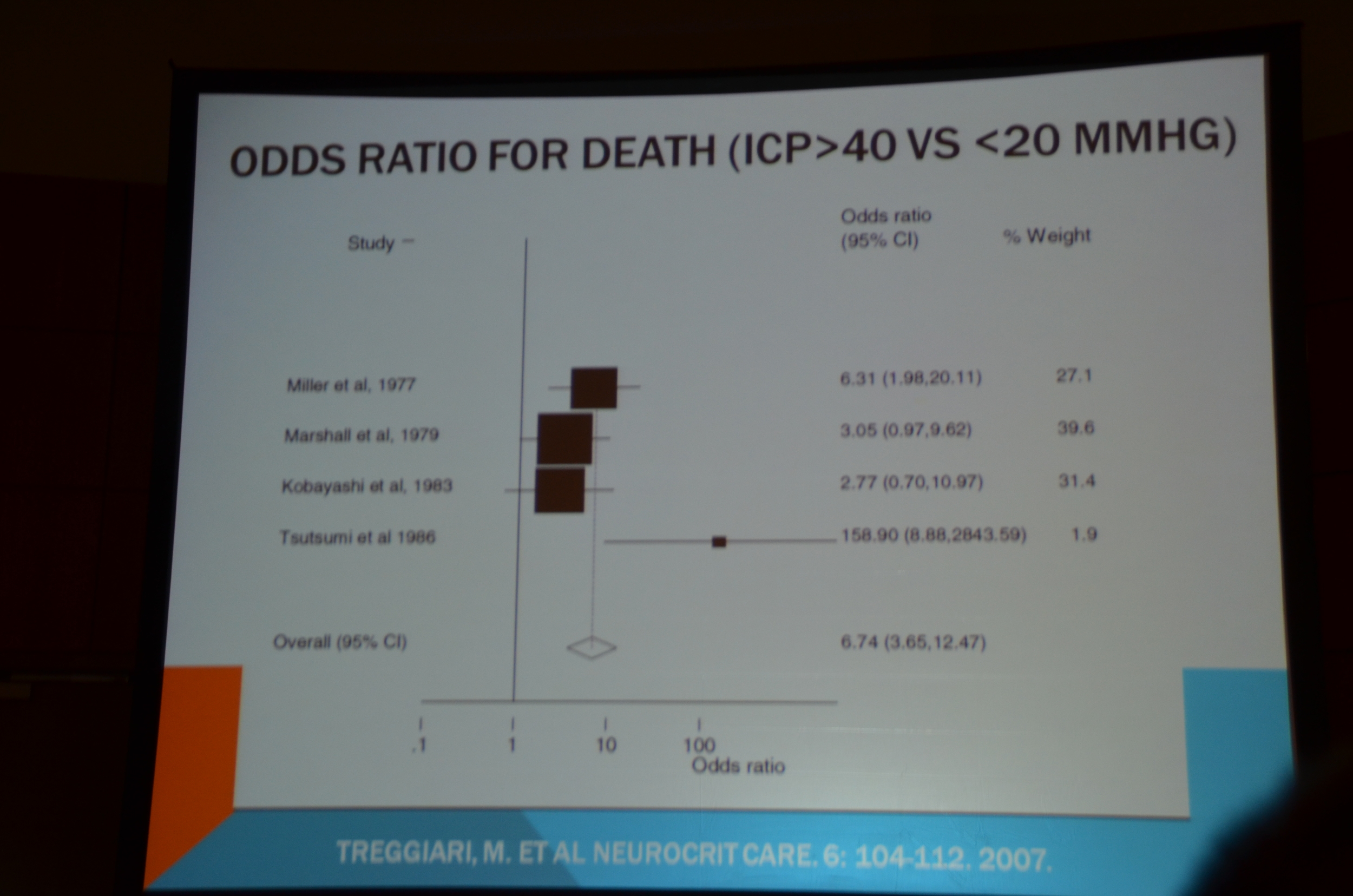
Dr. Berl then focused on the importance of maintaining cerebral blood flow, which is the product of cerebral perfusion pressure and vascular resistance. Cerebral perfusion pressure is the difference between systemic arterial pressure and intracranial pressure. You need to maintain cerebral perfusion pressure above 60 mmHg for good cerebral blood flow. He pointed to data that showed if the intracranial pressure was over 40 mortality was 56%, while below 20 mmHg it was only 18%.
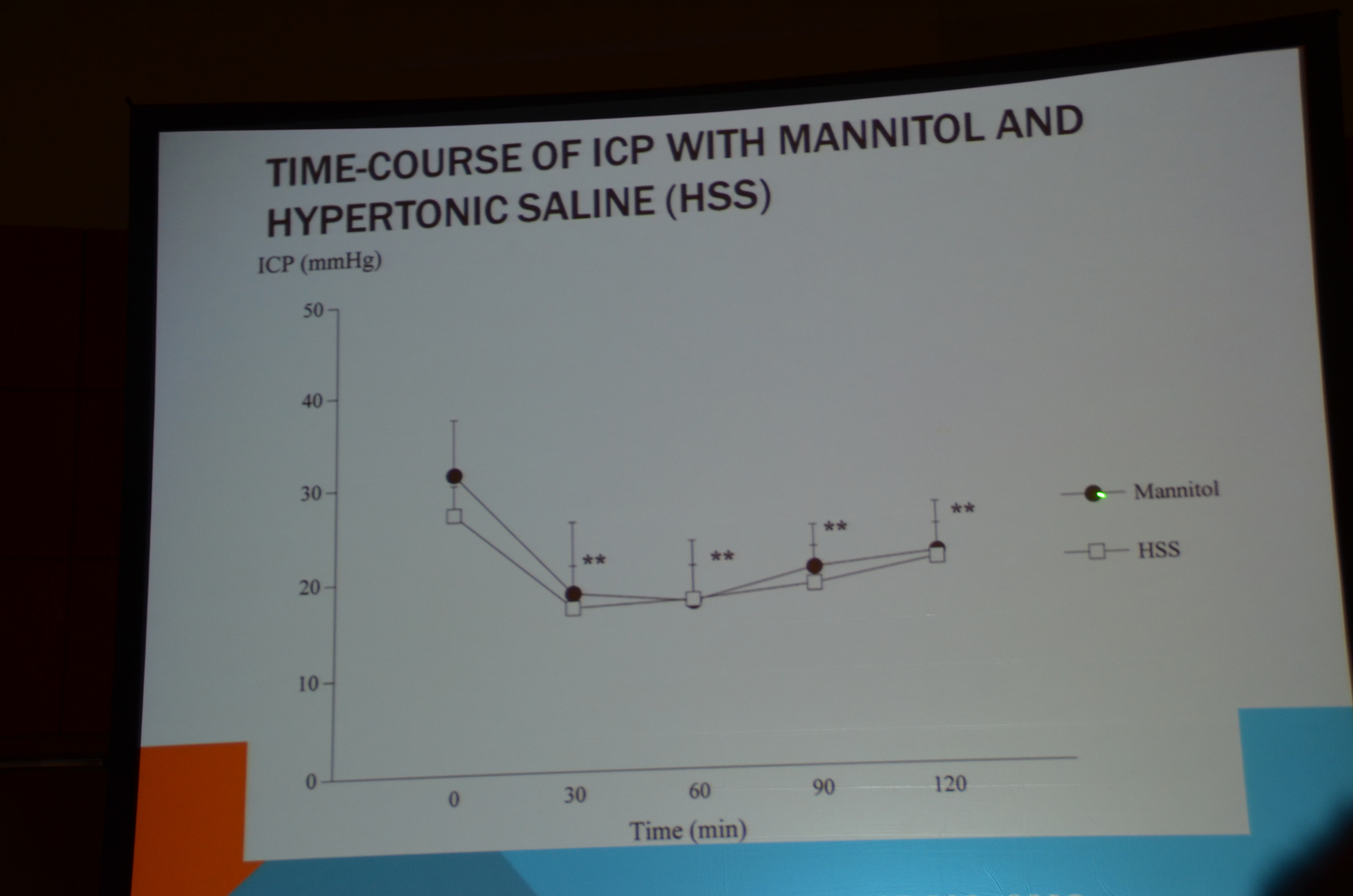
In order to control ICP focus on creating an osmotic gradient with mannitol or hypertonic saline.Koenig et al used 30 mL of 23.4% saline to lower the ICP by 40%, it raised serum sodium by 5 mEq/L. 30 mL of 23.4% is equivalent to 238 mL of 3%.
Berl summarized the interventions for improving cerebral perfusion pressure as the 3 Hs: hypervolemia, hypertension and hypertonicity. He added you could also do the fourth H, hyperventilation.
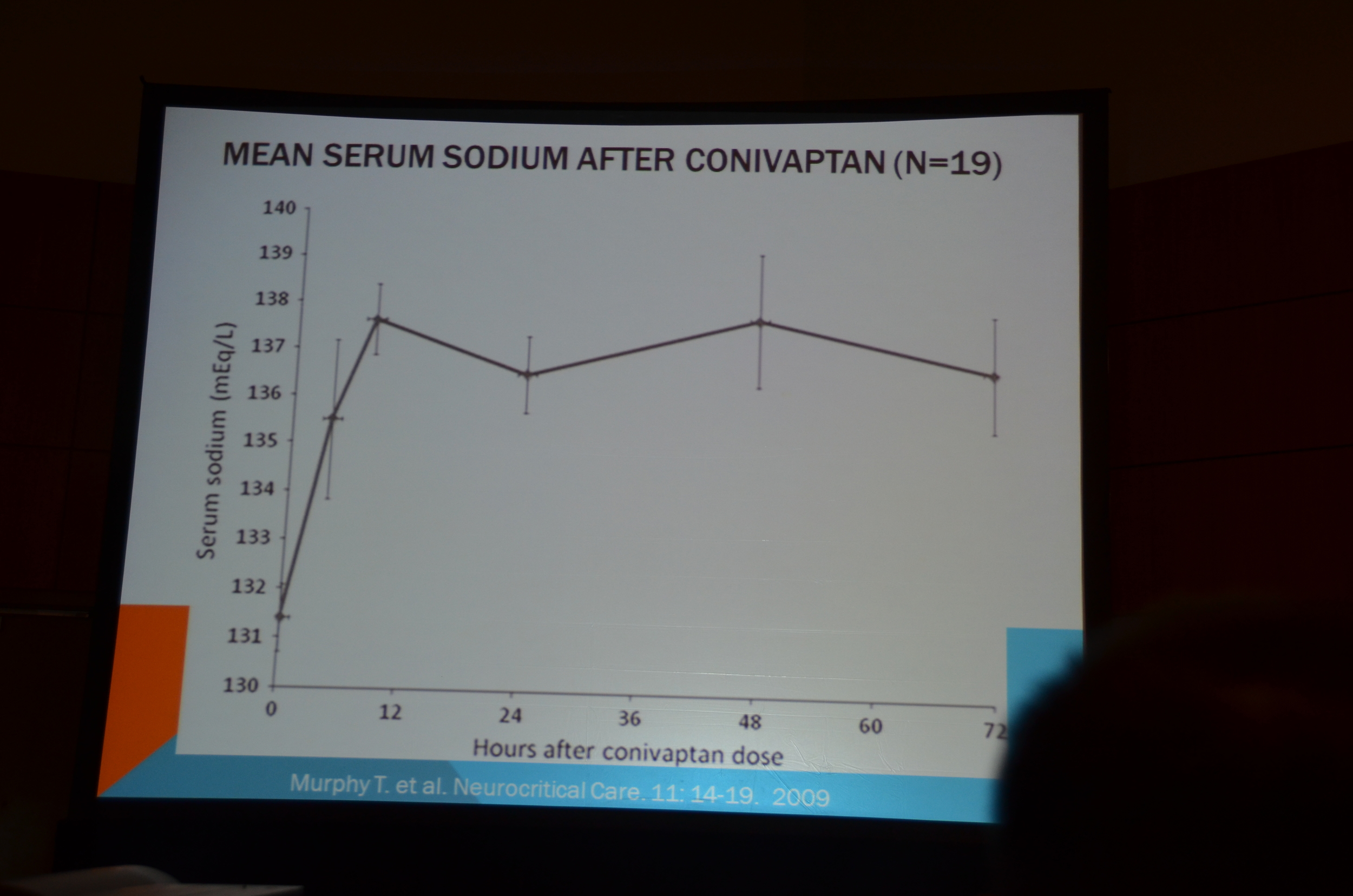
Hyponatremia is a complication often seen in neuro-ICU patients. Conivaptan has been used successfully and safely in this environment.
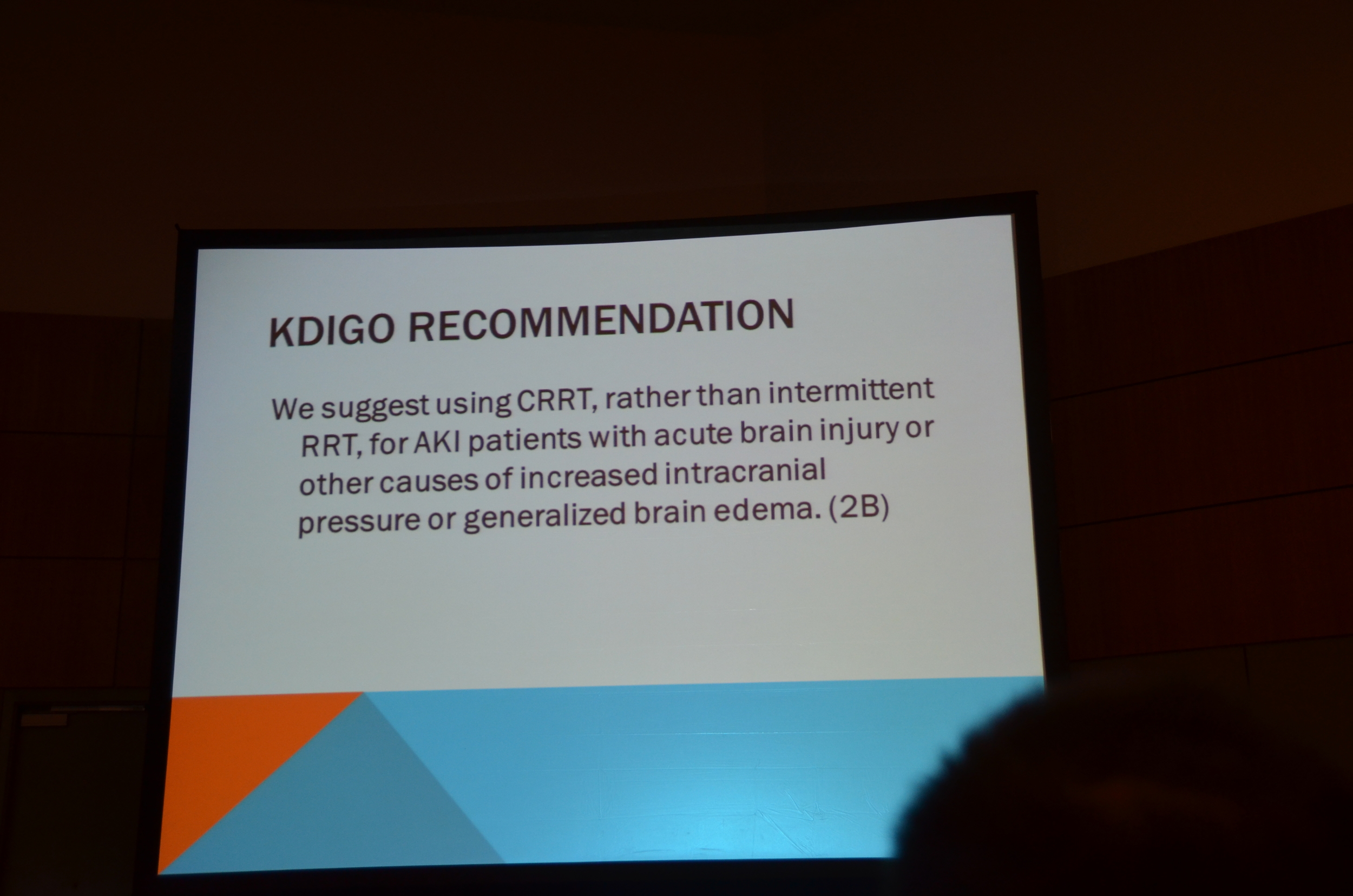
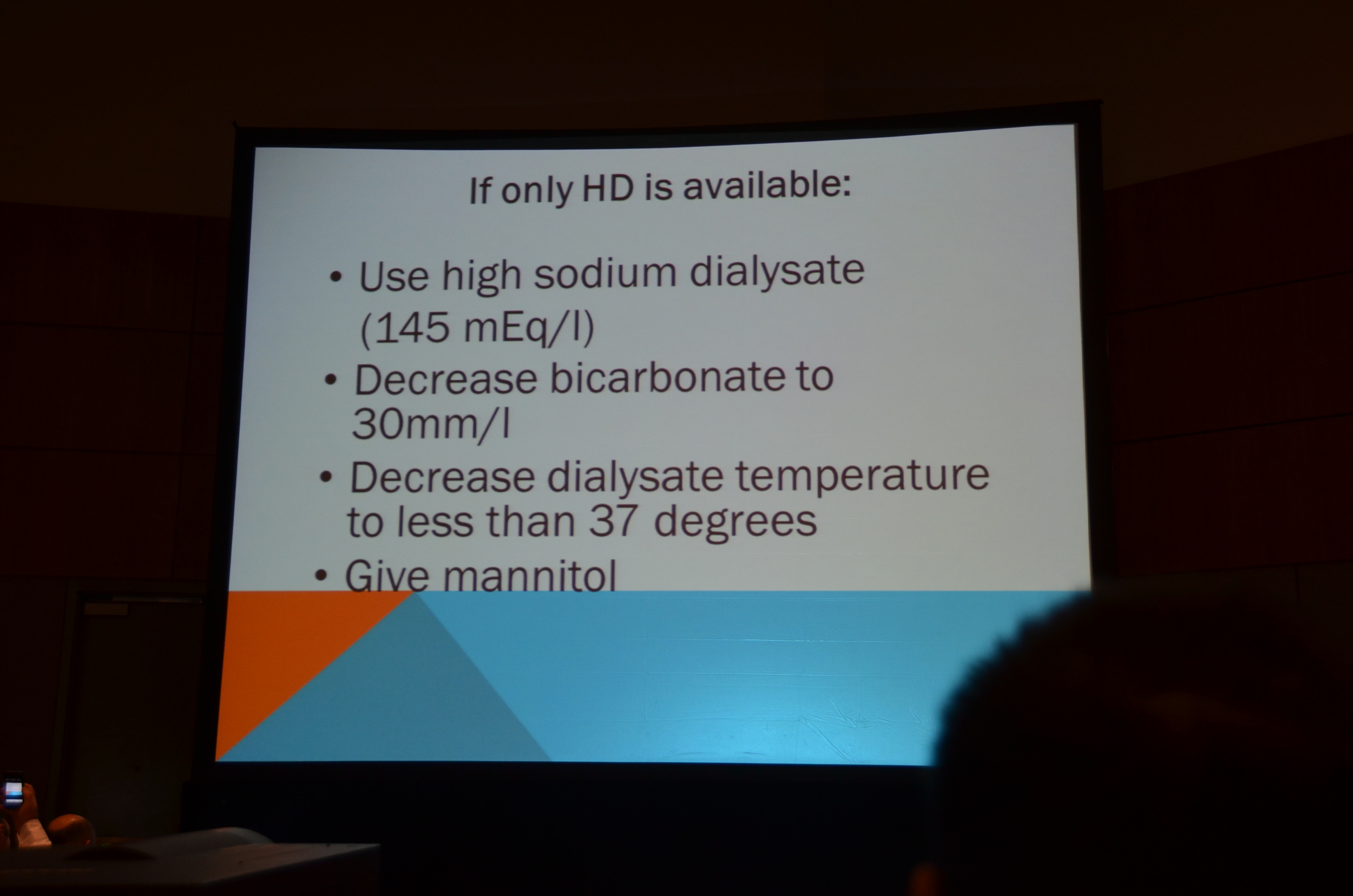
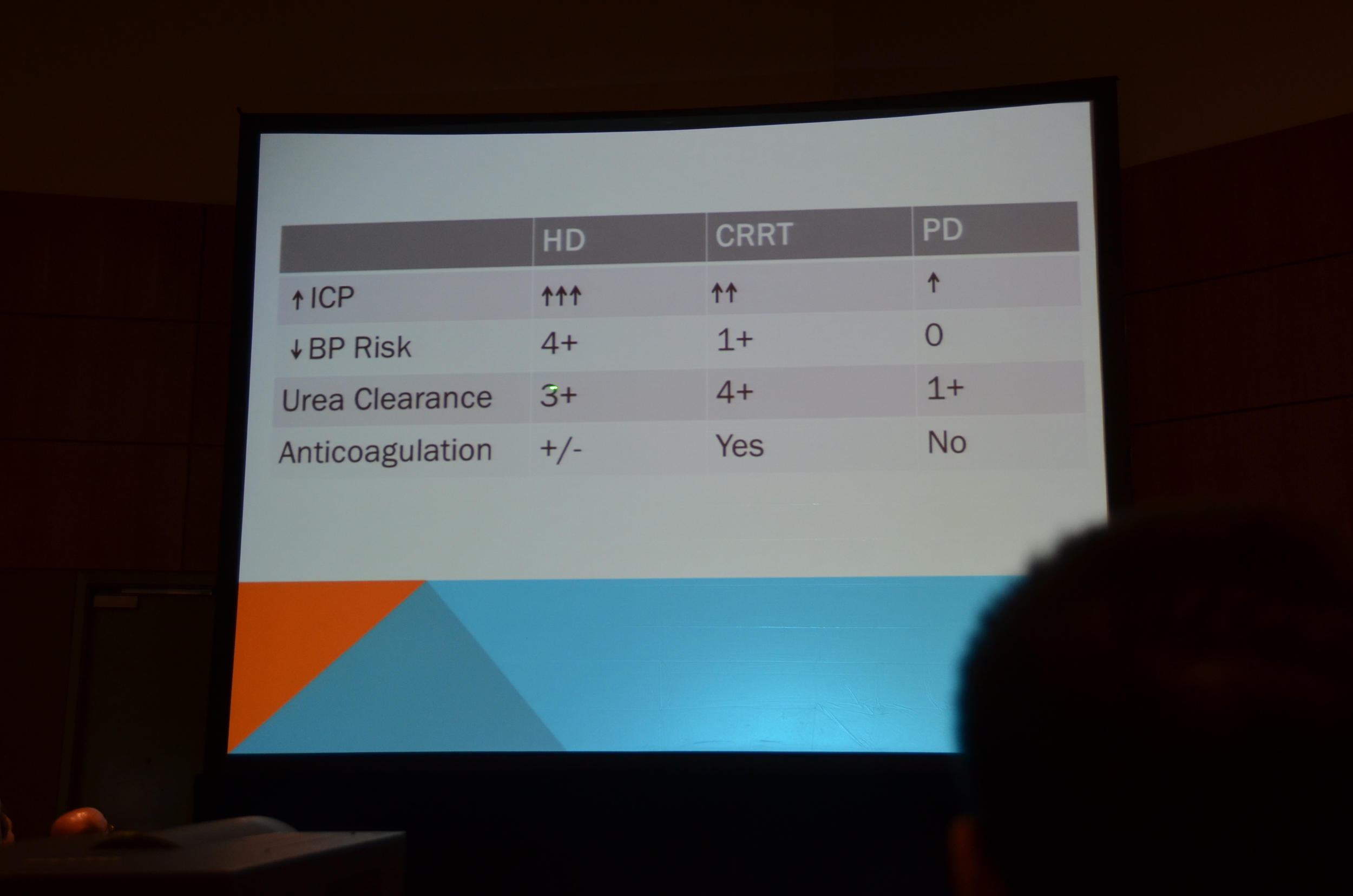
He concluded with mentioning the KDIGO recommendation for using CRRT rather than intermittent hemodialysis for patients with acute brain injury or other causes of increasedintracranial pressure.
My Live Tweet Stream
Ready to live tweet: Ward Rounds and AKI #KidneyWeek12
Sarah Faubel, my friend and co-author organized the talk. Sweet
#KidneyWeek12
First up is Neuro ICU
#KidneyWeek12
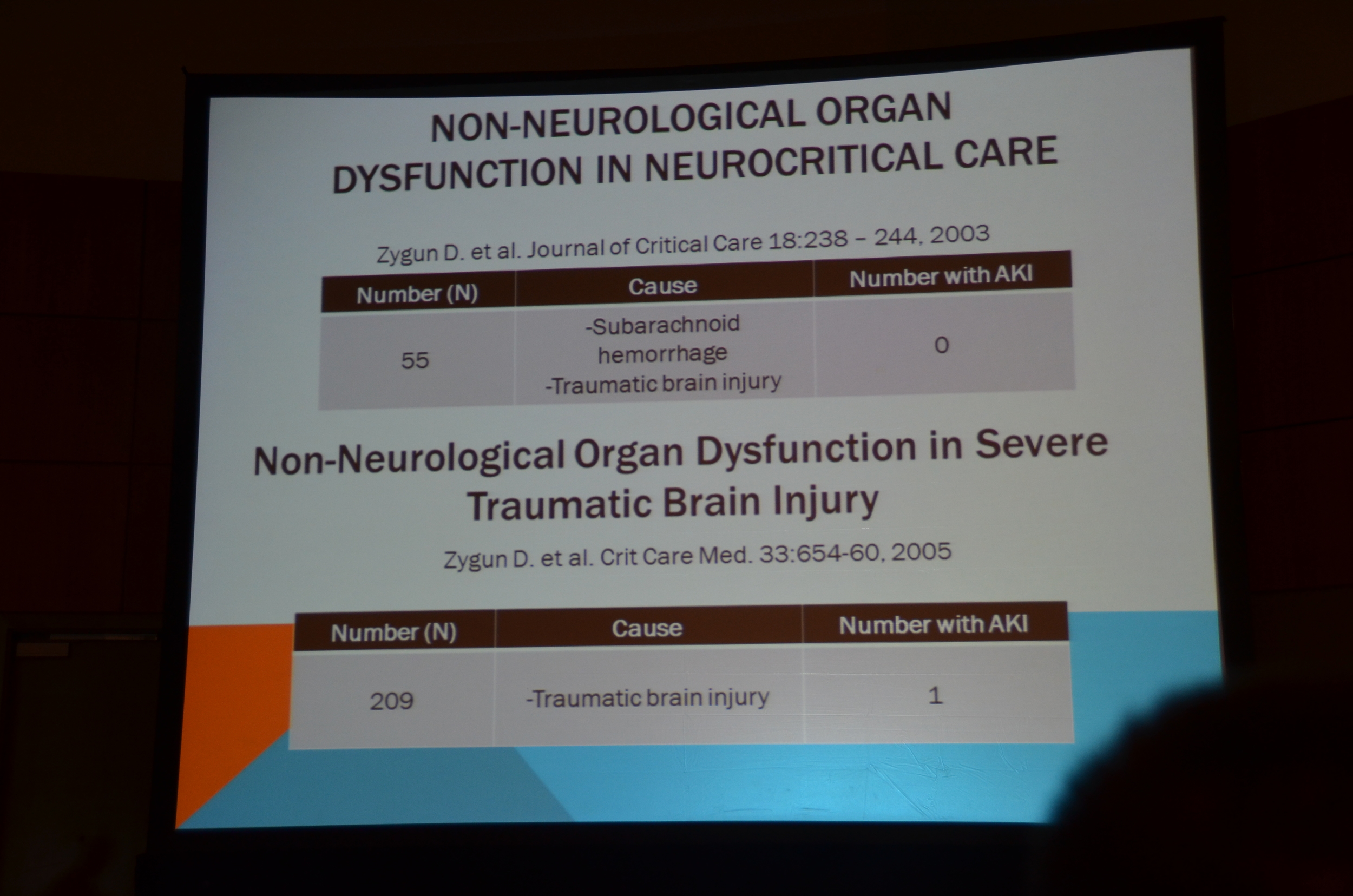
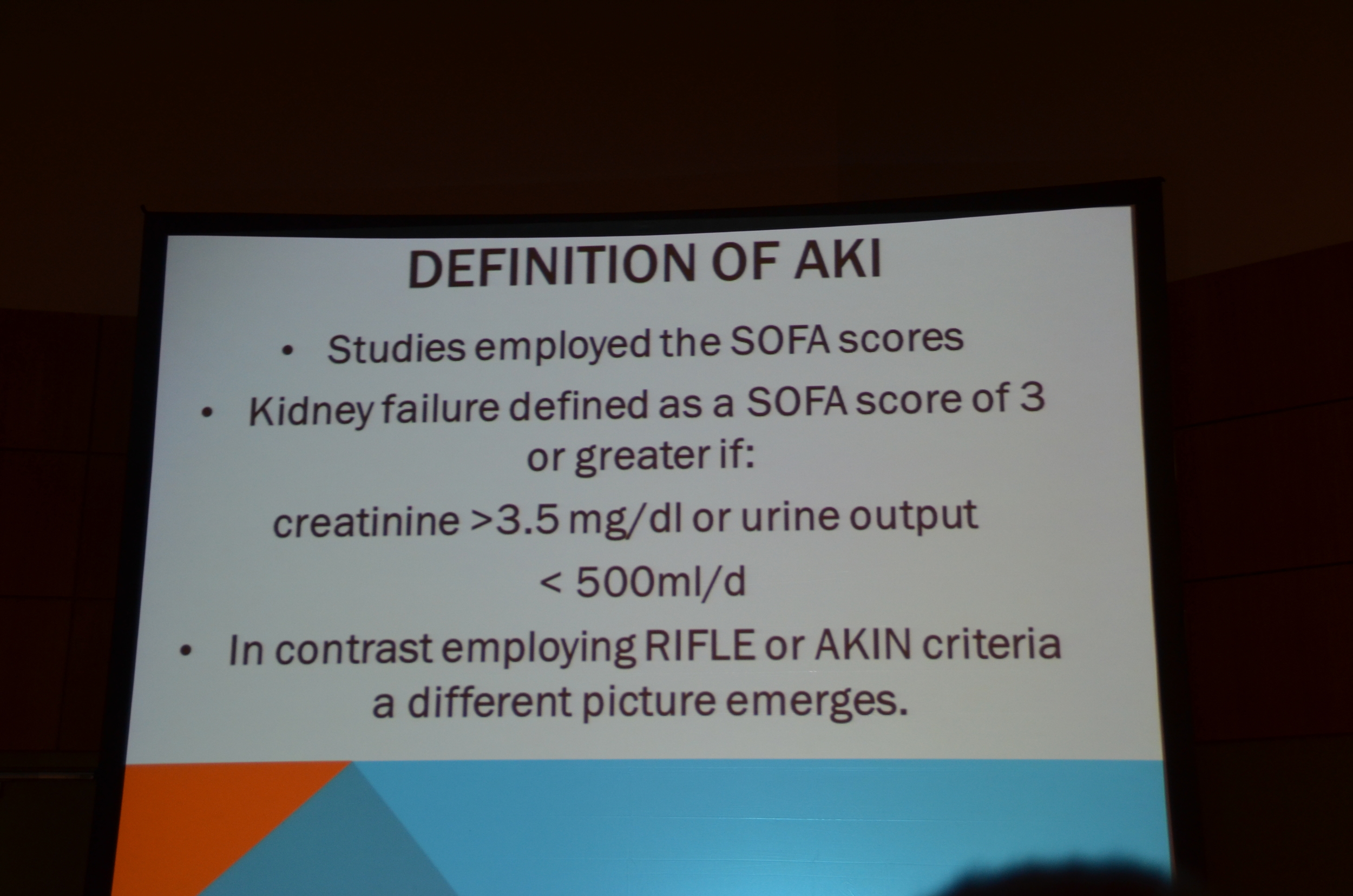
Zygun Crit Care 2005 surveyed 209 patients. Used Cr of >3.5 of UO < 500/day #KidneyWeek12
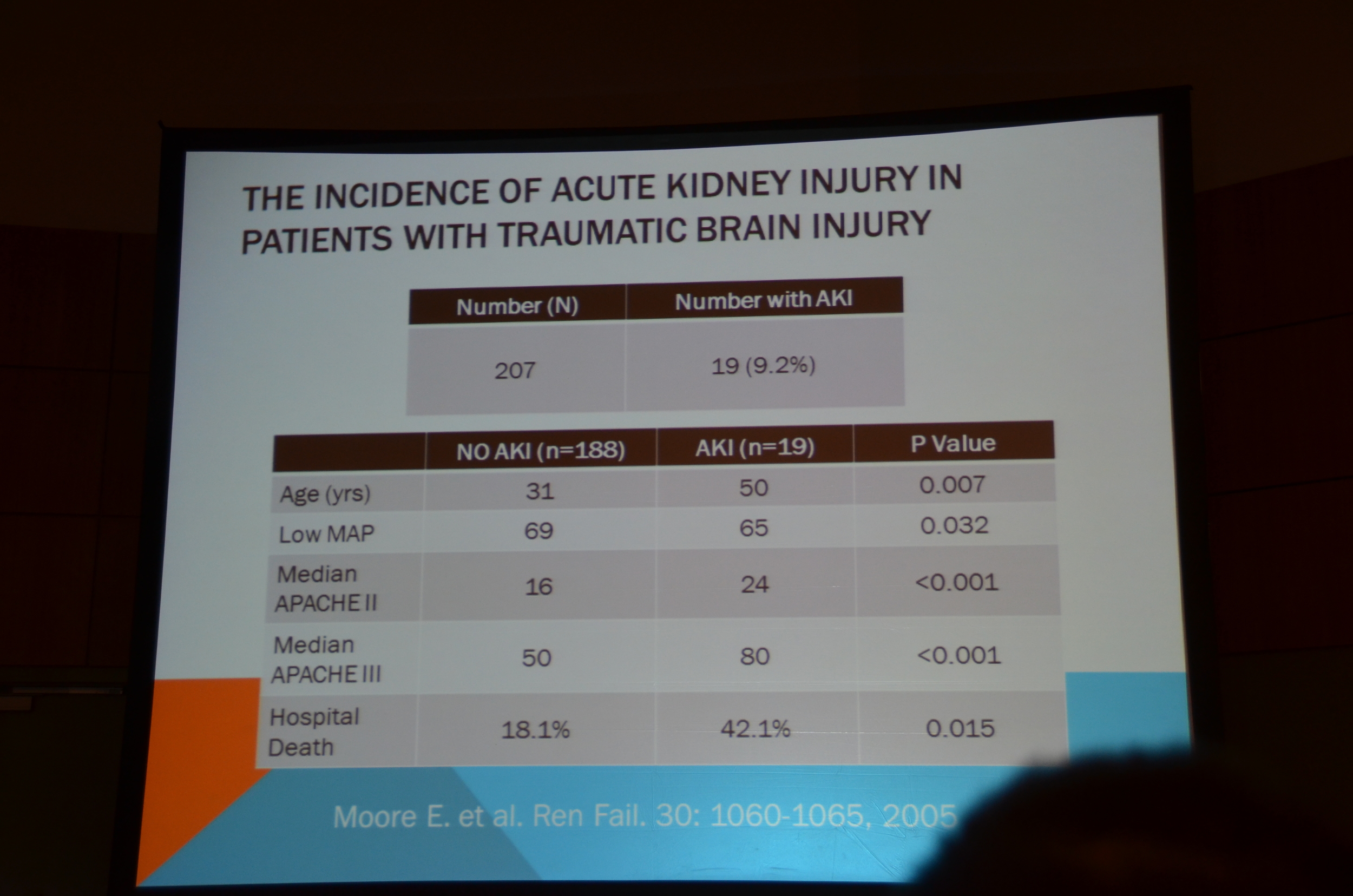
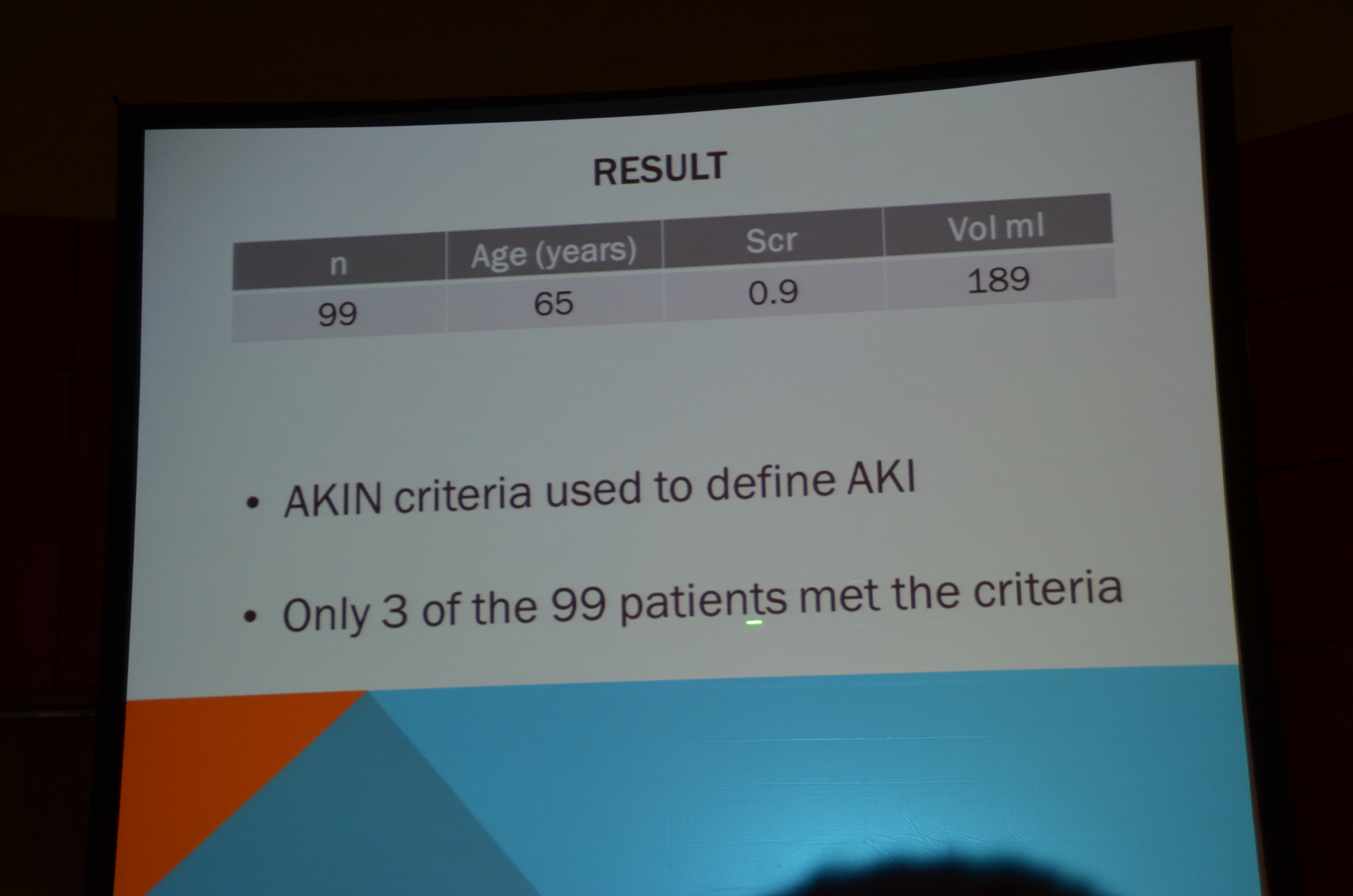
Moore in Renal Failure 2005 using AKIN Criteria found 9.2% with AKI. #KidneyWeek12
AKI raised mortality from 18 to 42% (Moore data) #KidneyWeek12
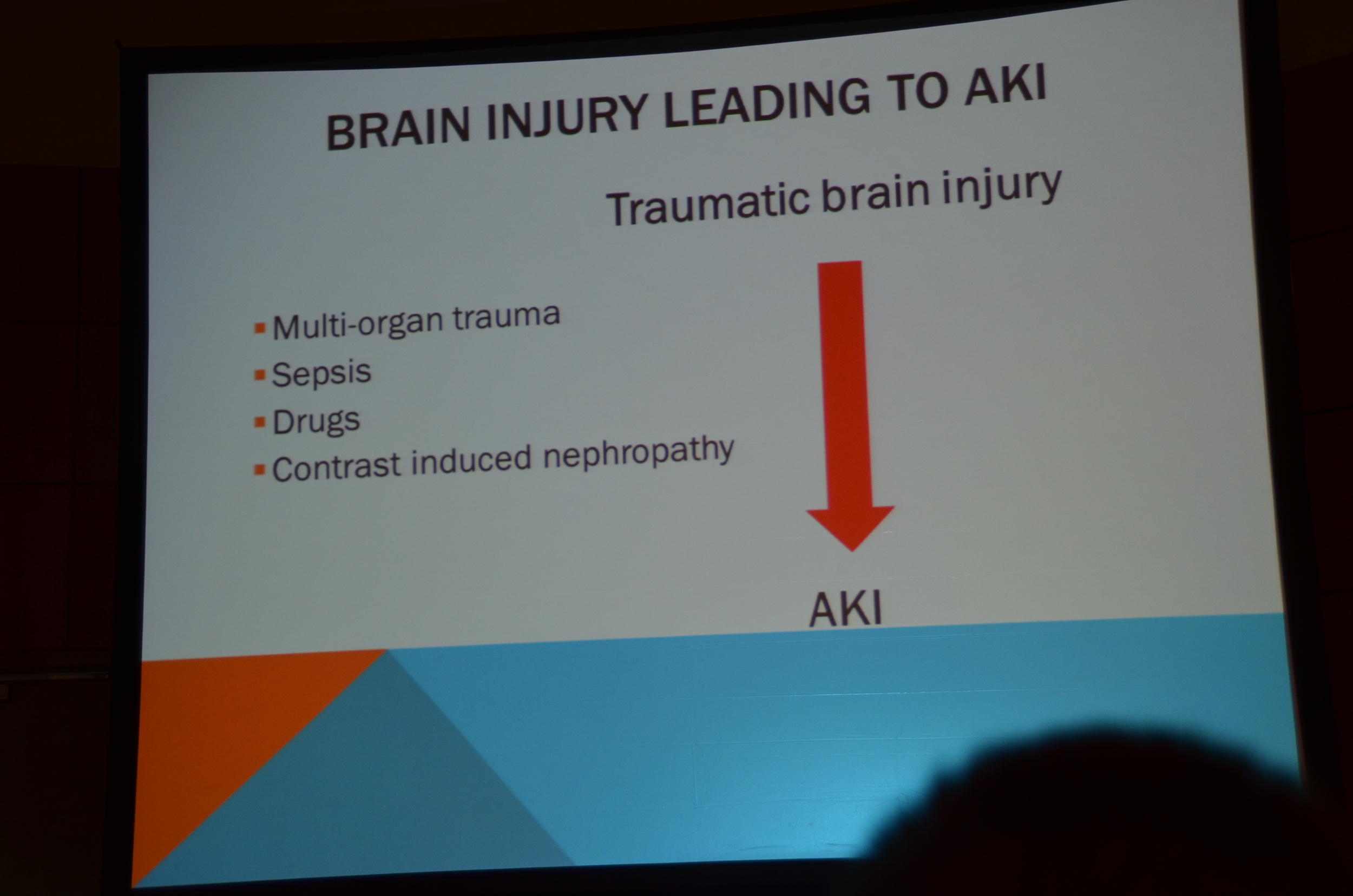
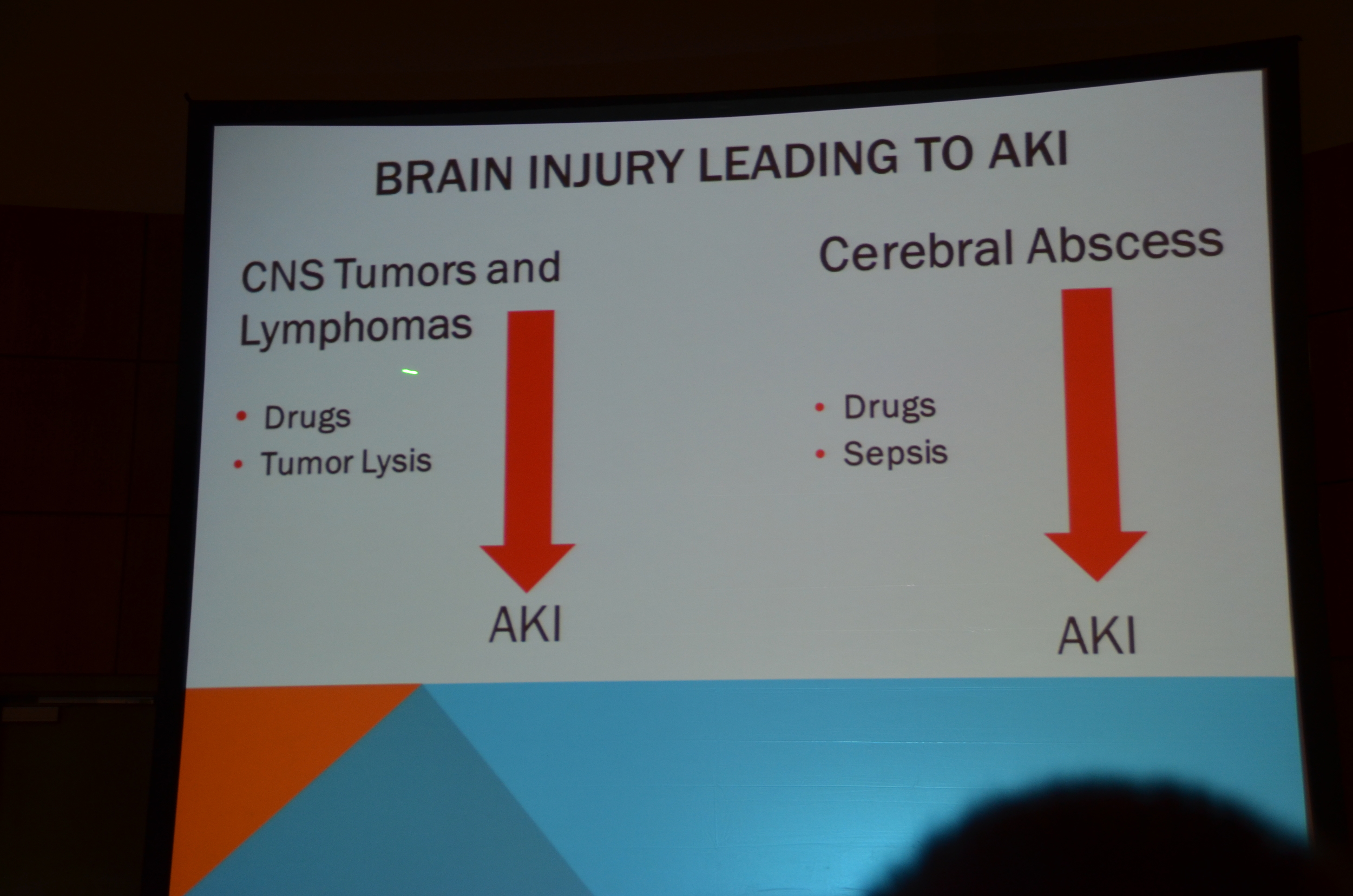
Multi-organ failure, sepsis, drugs and contrast all lead to AKI in neuro ICU #KidneyWeek12
Incidence of contrast nephropathy in neuro-surg patients (Cr up 25% or 0.5 mg/dL)23% in 92 pts with mean GFR of 98. #KidneyWeek12
No difference in risk with low or iso-osmolar contrast.
sarafin ACTA Radiollogica 52 2011. #KidneyWeek12
Second study, I didn't catch the ref, found a rate of only 3% contrast nephropathy in neuro ICU. More believable. #KidneyWeek12
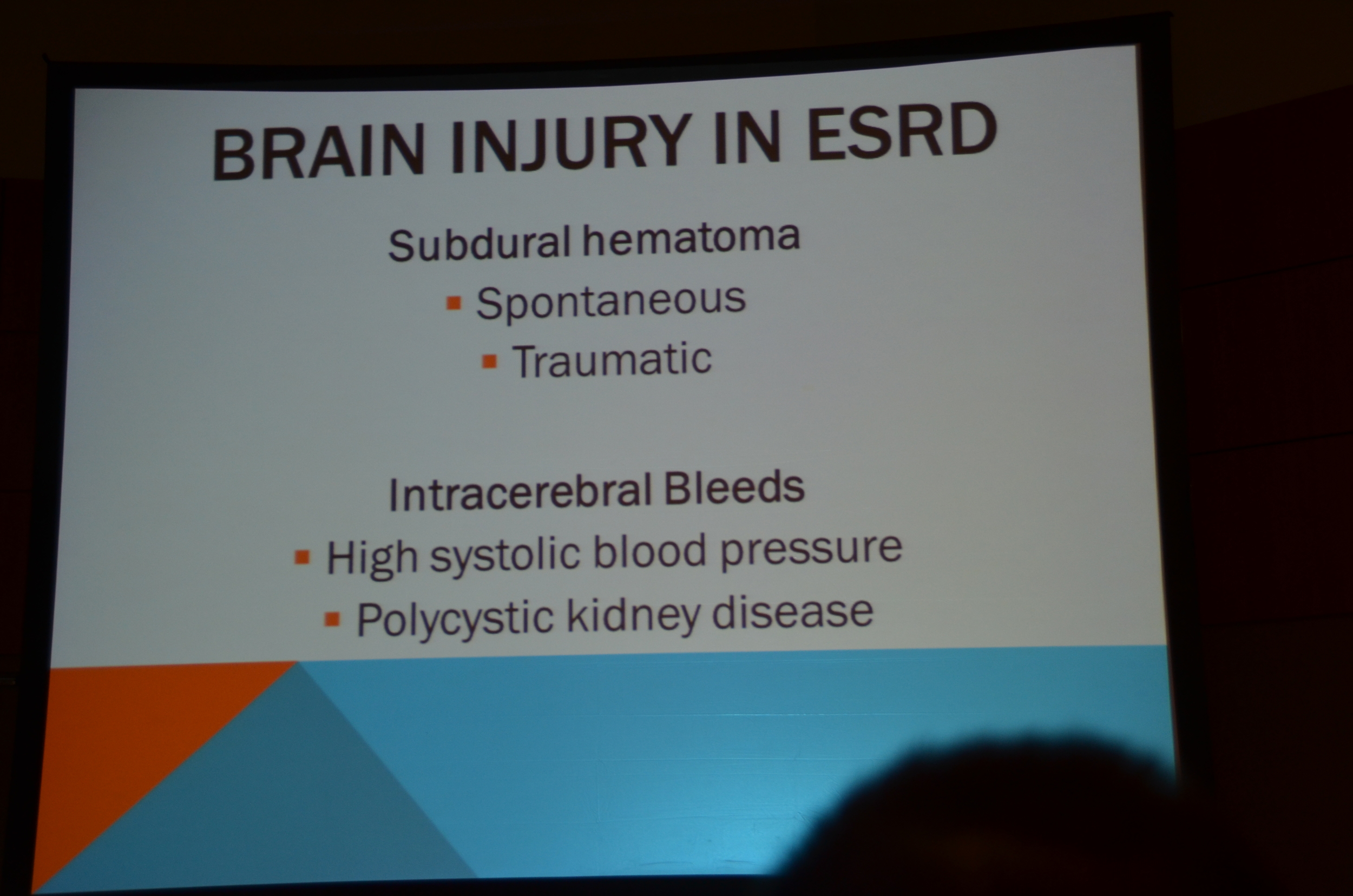
Subdural hematomas, more common in ESRD. #KidneyWeek12
Center piece of management in maintenance of cerebral blood flow #KidneyWeek12
Goal cerebral perfusion pressure is 60 mmHg #KidneyWeek12
Recommends NEJM review: 367 2012. (http://www.nejm.org/doi/full/10.1056/NEJMct1206321)
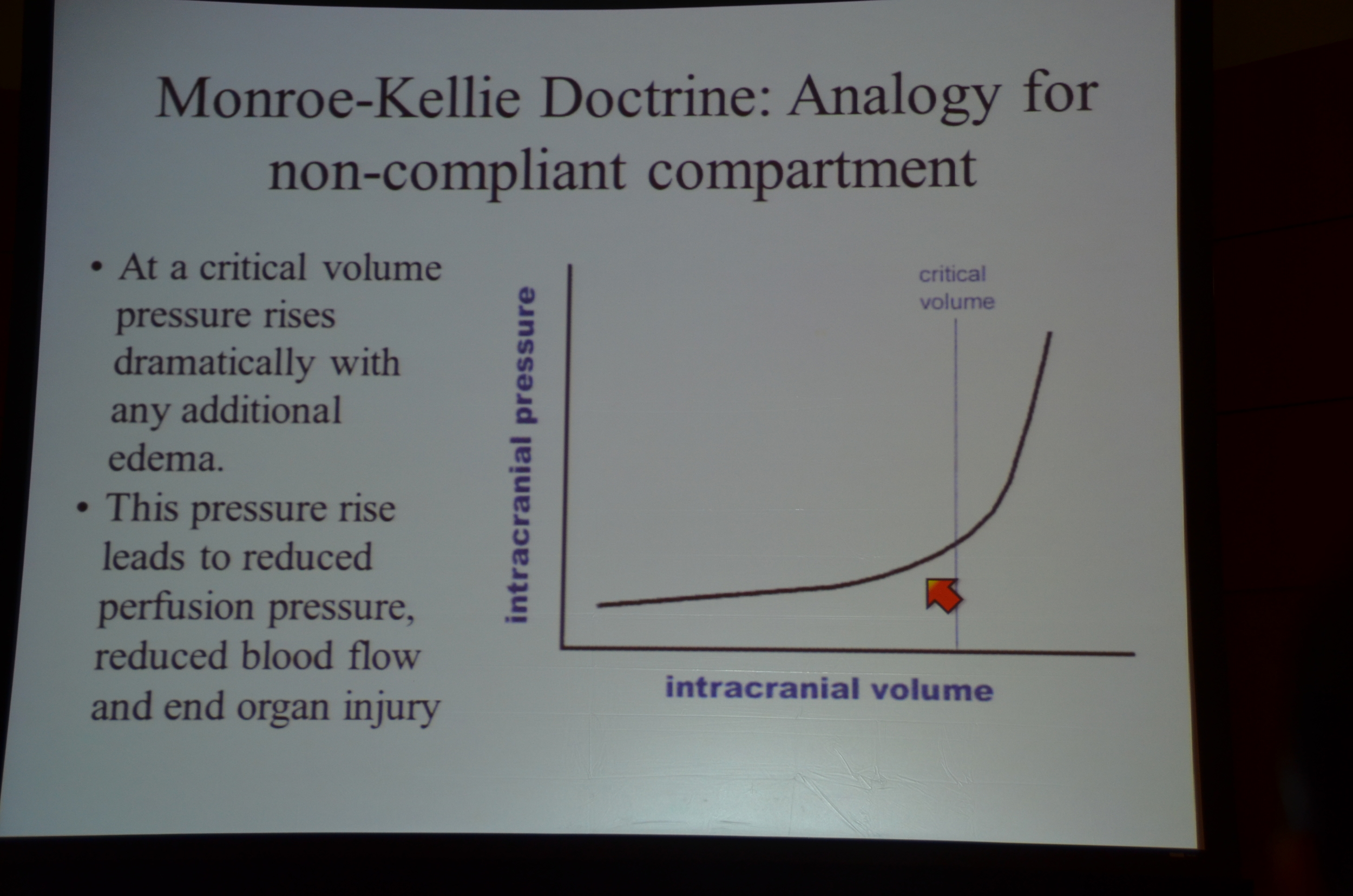
ICP is dependent on intracranial volume #KidneyWeek12
If ICP goes over 40 mmHg mortality goes way up 20->40%). Treggiari Neurocrit care 2007 #KidneyWeek12
Koenig Neurology 70 2008. Used hypertonic 23.4% NaCl 30 ml (equiv of 238 ml of 3%) increased Na by 5, decreased ICP by 40% #KidneyWeek12
Conivaptan for hyponatremia in the neuro ICU. Murphy T Neurocritical Care 2009. Na up 5.8 mEq/L in 12 hours. No CPM. #KidneyWeek12
To improve cerebral perfusion pressure the 3 or 4 H's:
Hypervolemia
Hypertension
Hyperosmolality
and maybe Hyperventilation #KidneyWeek12
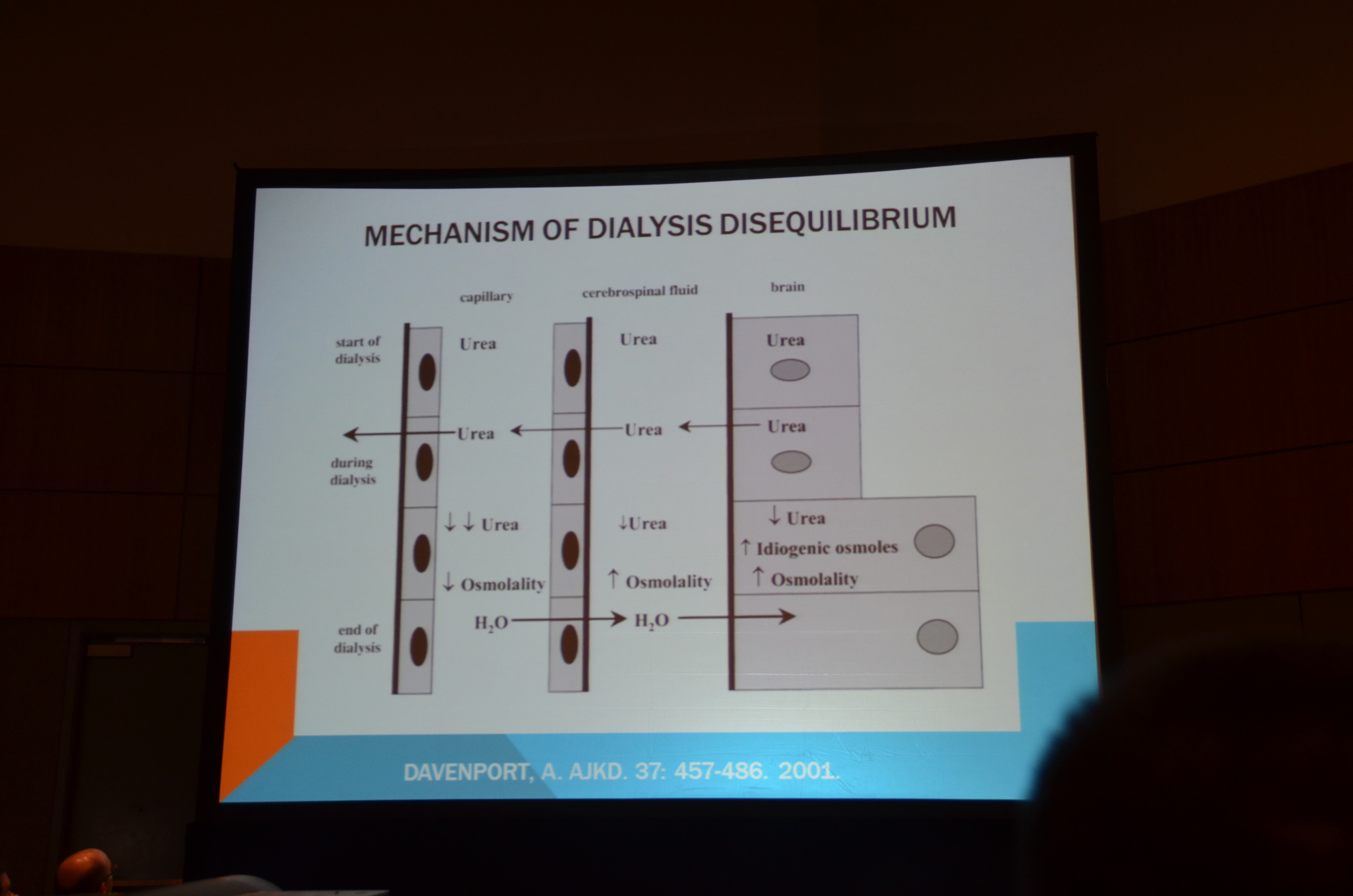
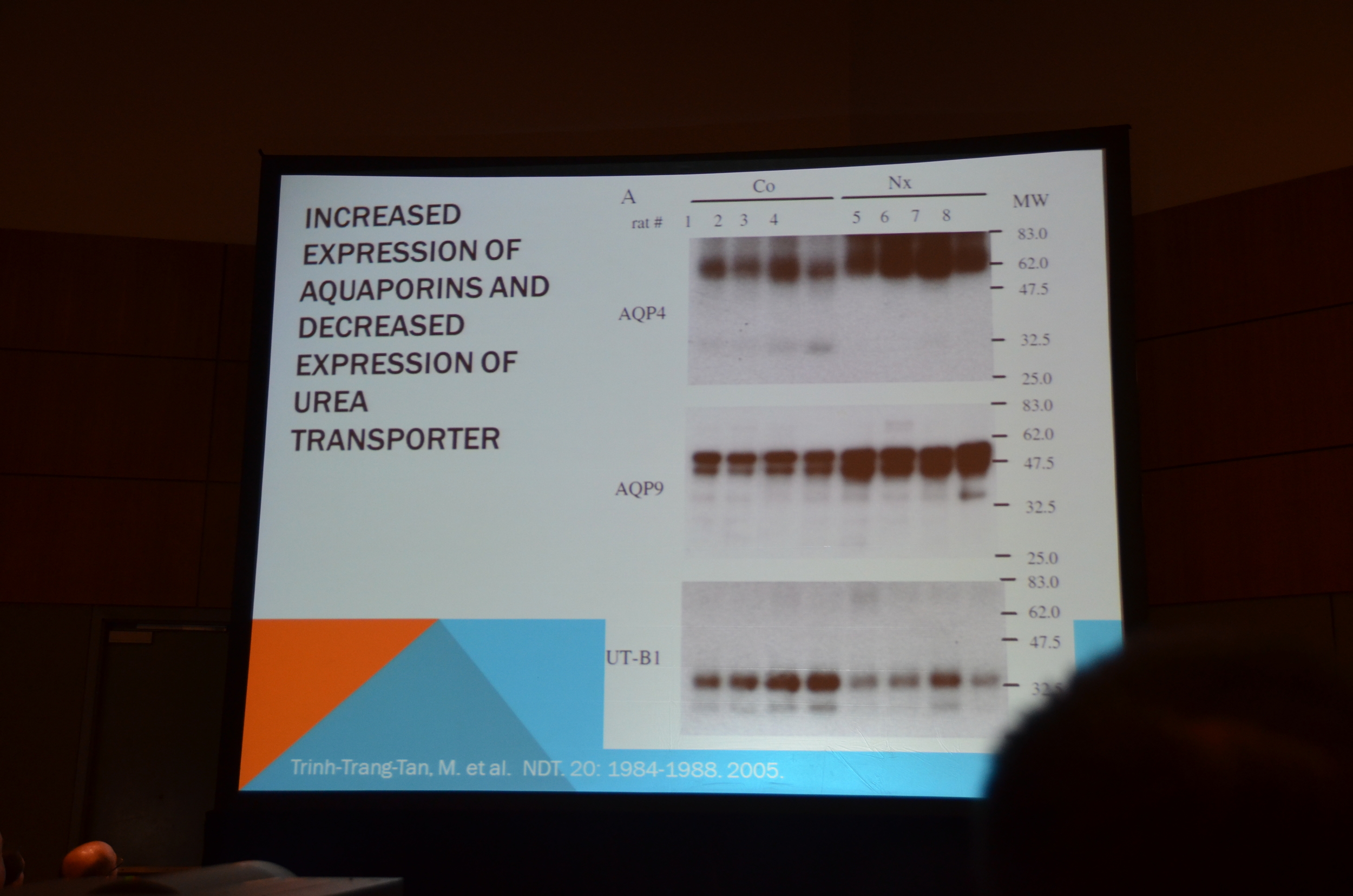
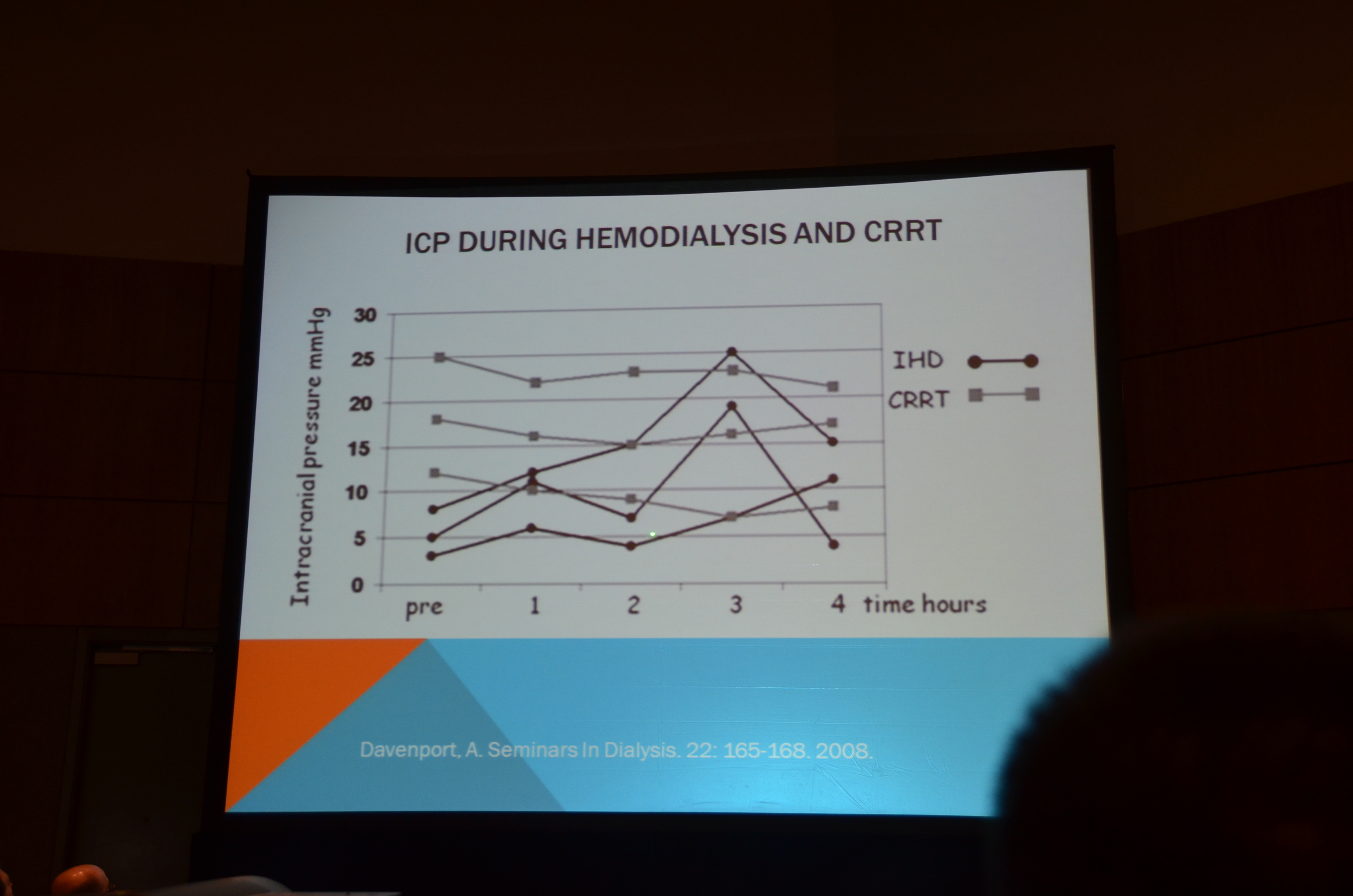
KDIGO recs CRRT not intermittent HD to stabilize ICP. IHD: much less stable ICP. davenport seminars in dialysis 2008 #KidneyWeek12
Trauma
Trauma
Lakhmir S. Chawla







My post in eAJKD
Kidney Week 2012: AKI in the Trauma ICU
The second lecturer was Lakhmir Chawla, MD of George Washington University, talking about AKI in the Trauma ICU.
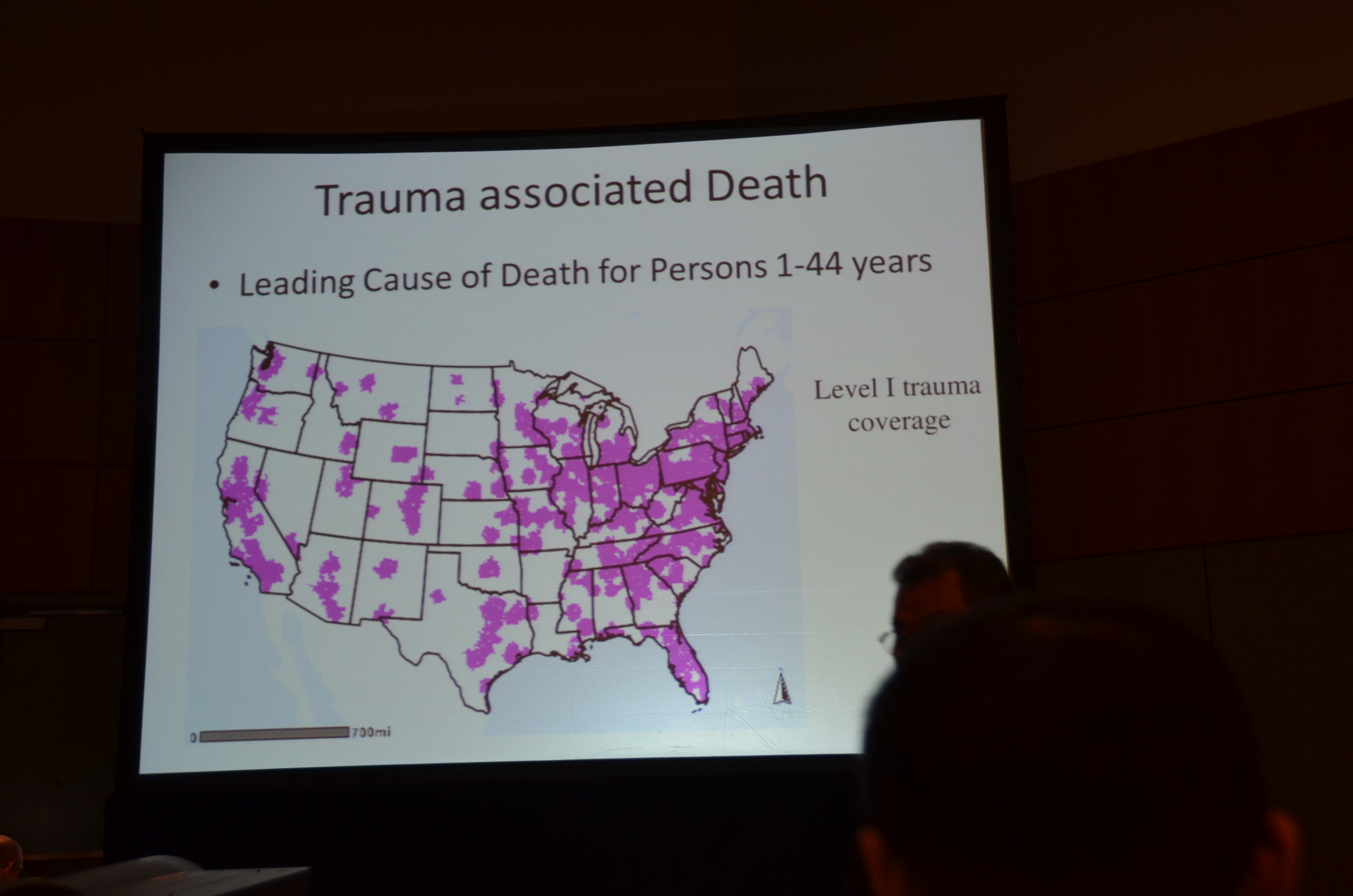
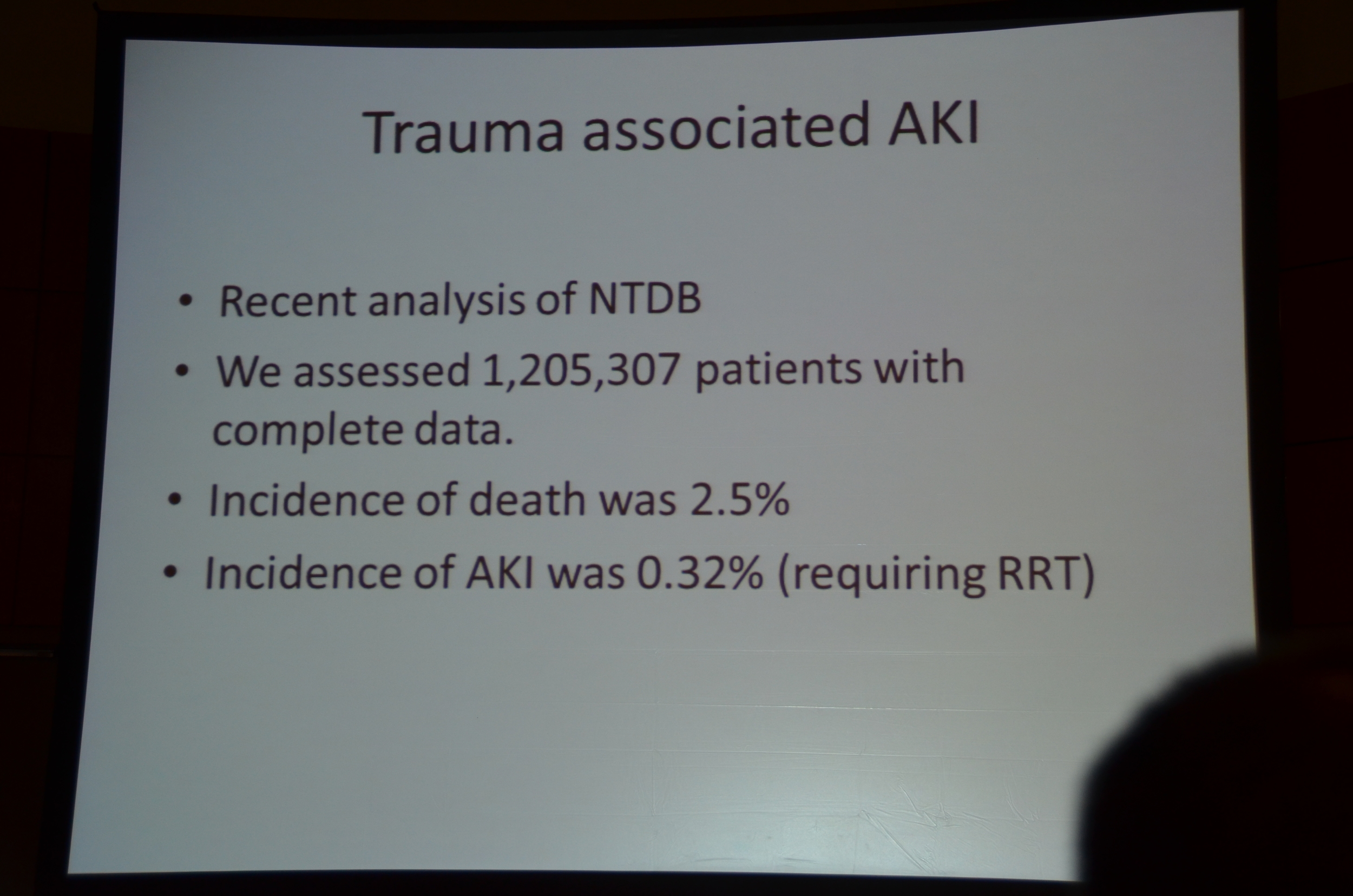
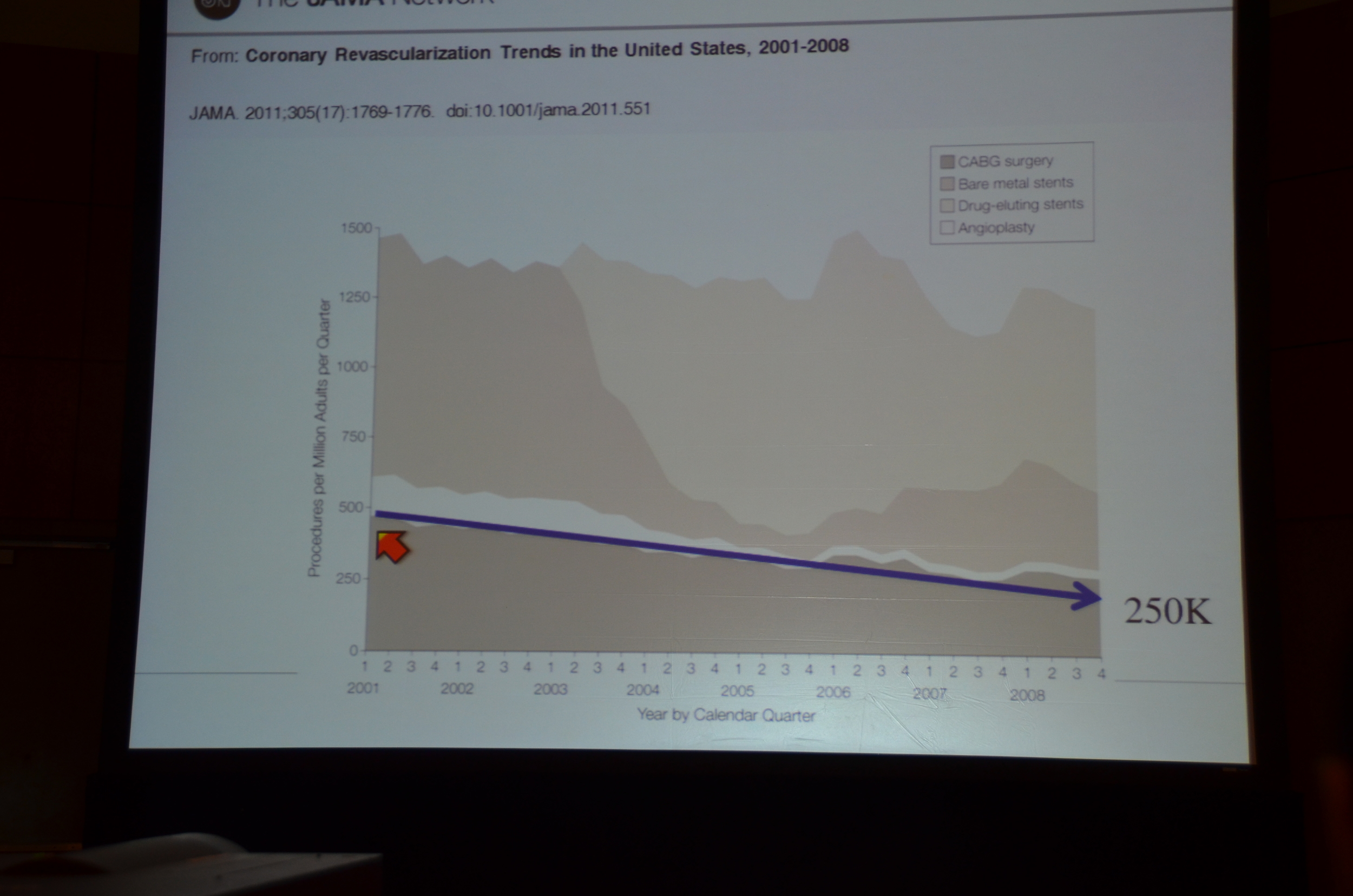
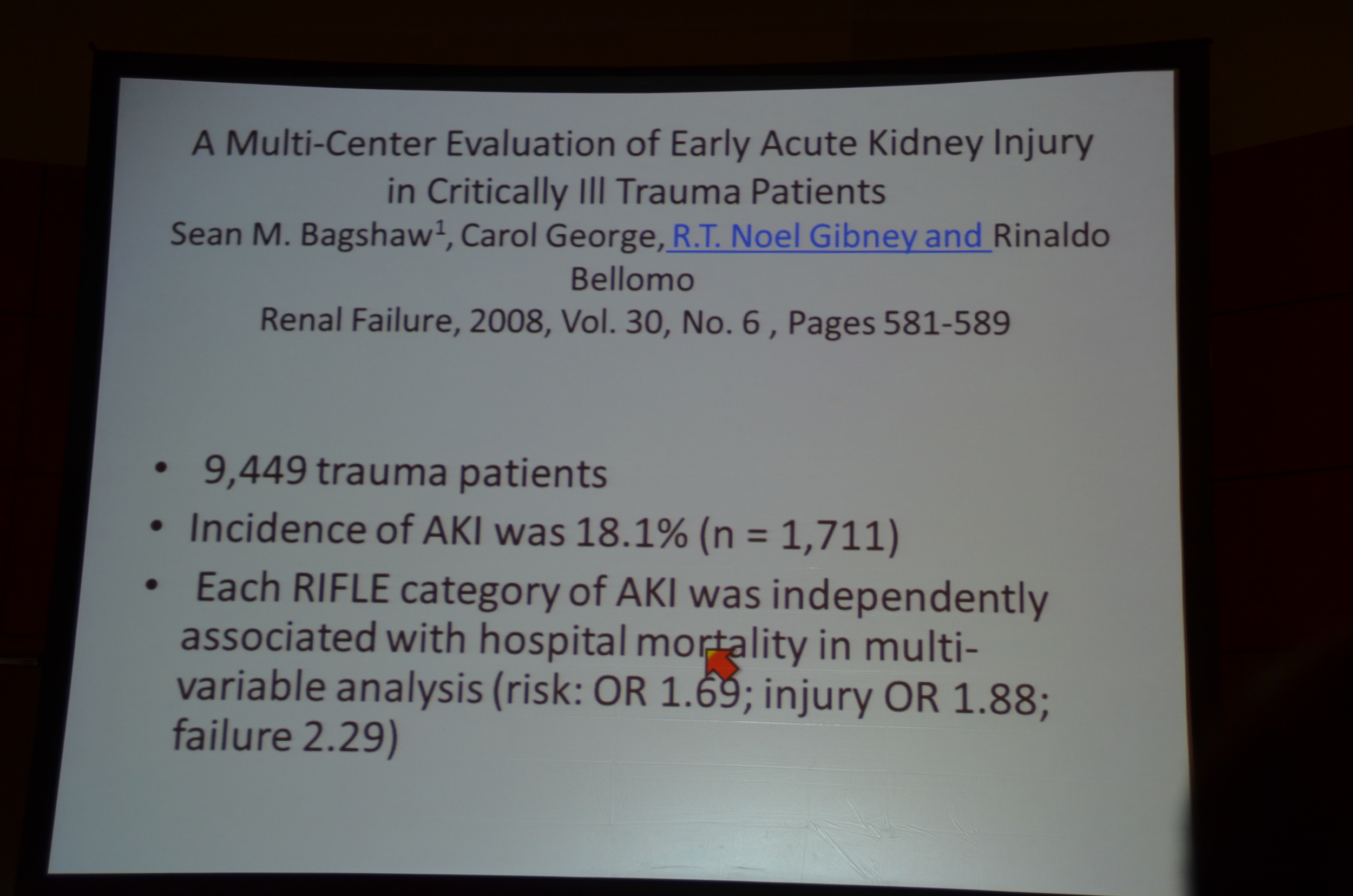
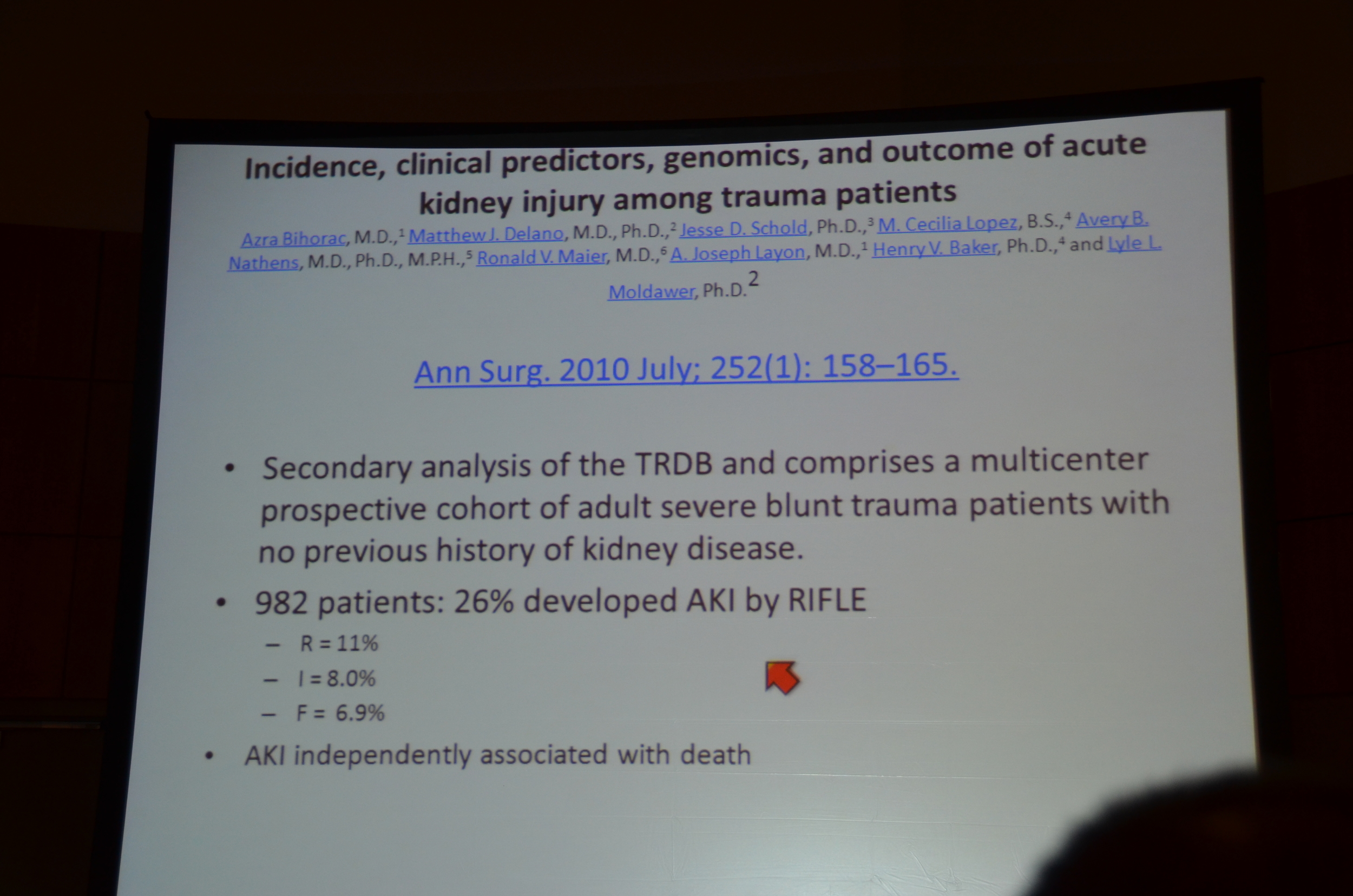
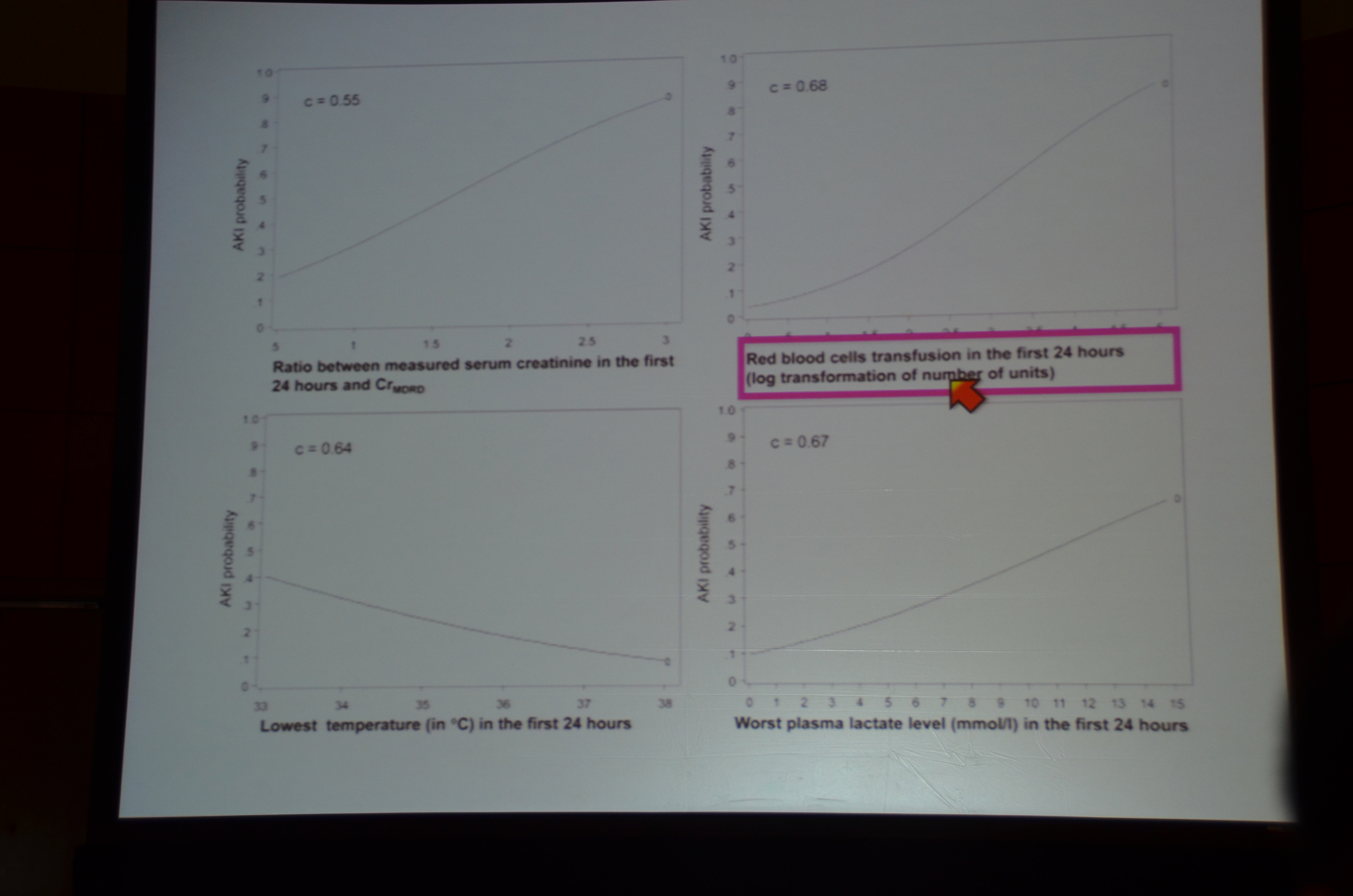
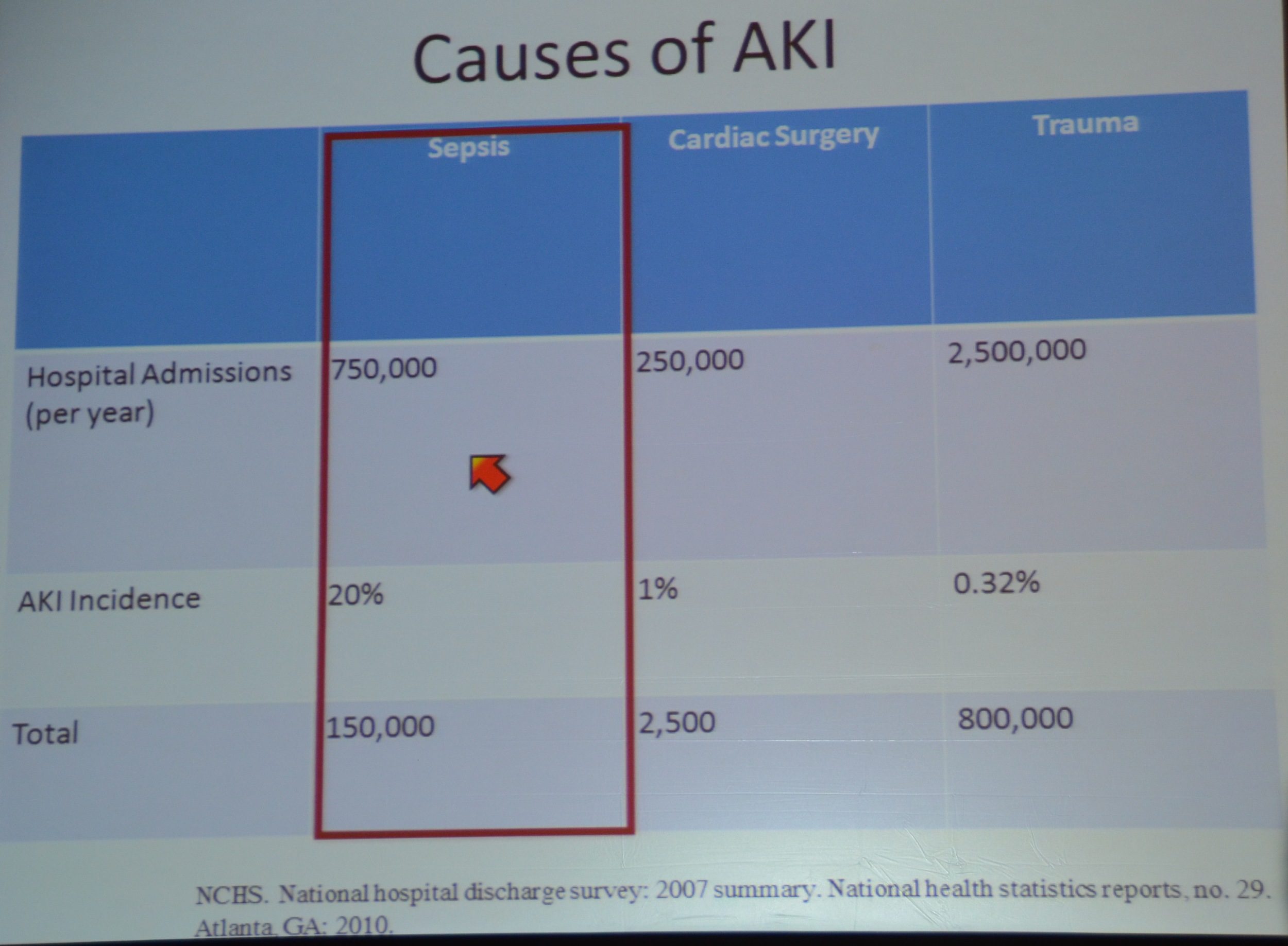
Trauma is the leading cause of death for patients aged 1-44 years.AKI occurs in 0.32% (this is dialysis dependent AKI, and his own, unreferenced data). Given the frequency of trauma this represents a significant incidence of acute kidney injury. Dr. Chawla references data from theNational Hospital Discharge Survey in 2007 that identified 2.5 million admissions for trauma. If his data on the rate of dialysis dependent AKI holds up, that translates into 8,000 cases of dialysis dependent AKI, compare that to the 2,500 cases due to cardiac surgery. He then pointed to a survey of blunt trauma patients who had an incidence of AKI of 26% by RIFLE criteria:
R = 11%
I = 8.0%
F = 6.9%
Poorly resuscitated patients more commonly suffered from AKI, which was identified as an independent predictor of death in trauma patients.
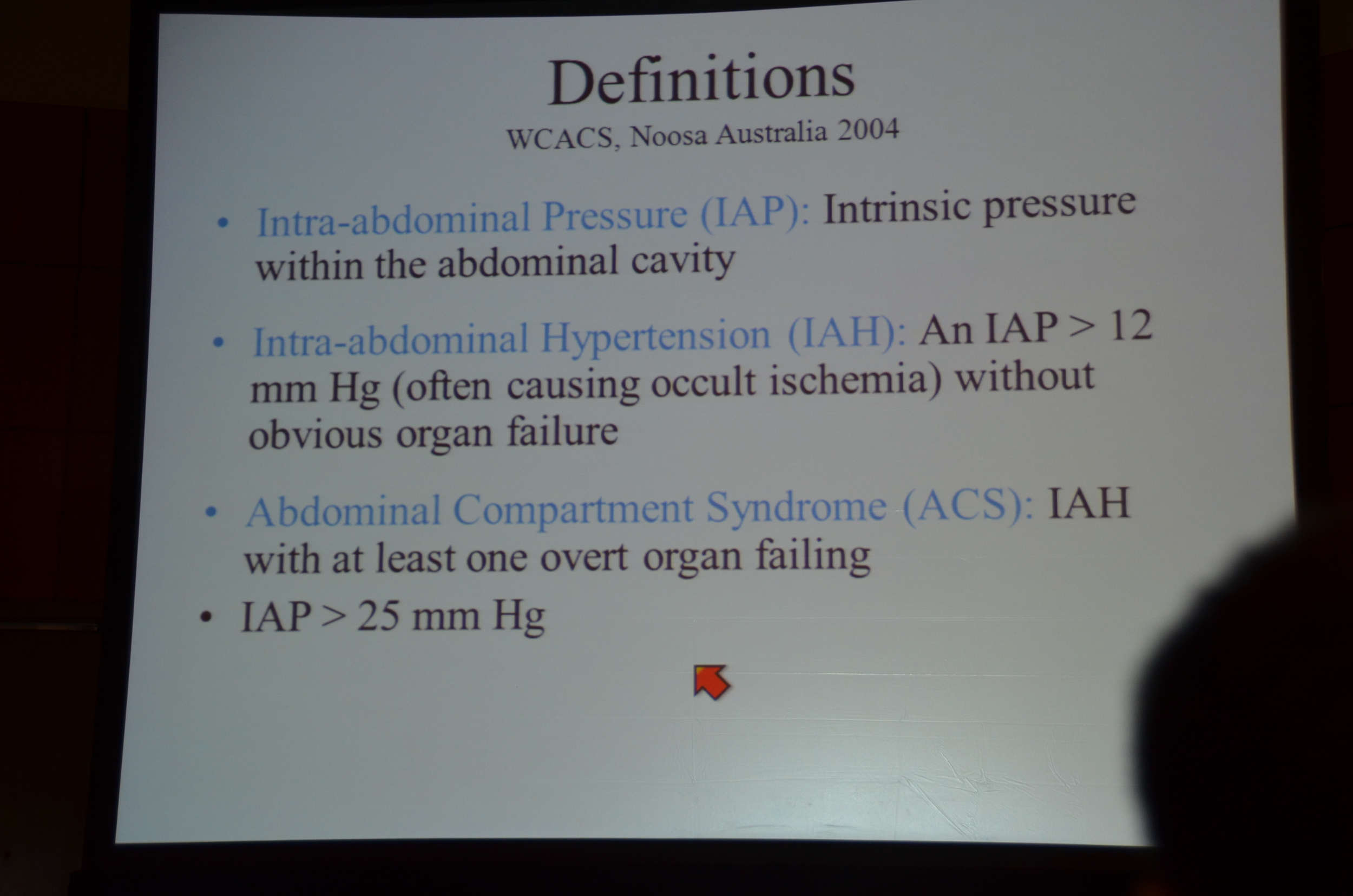
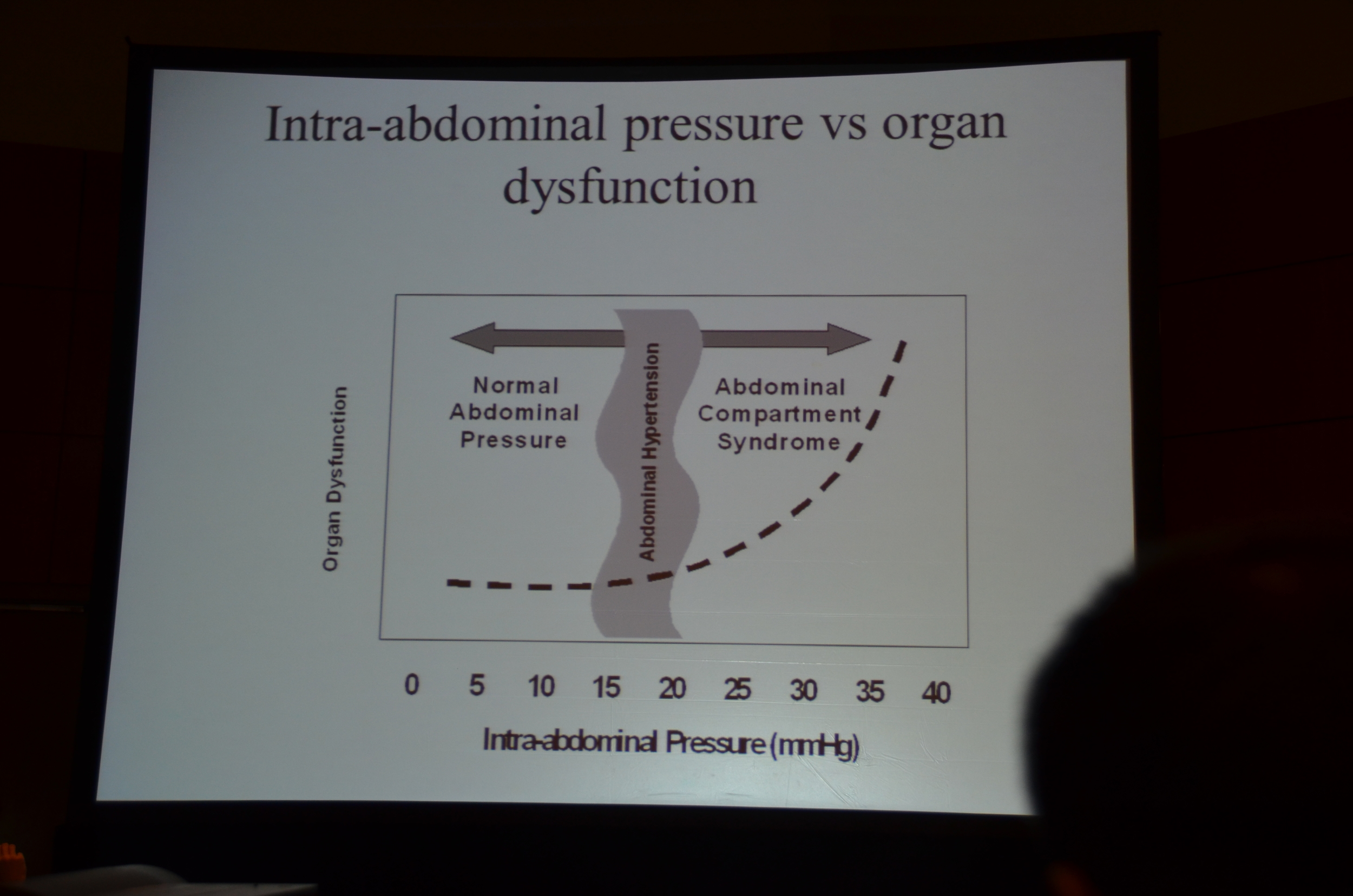
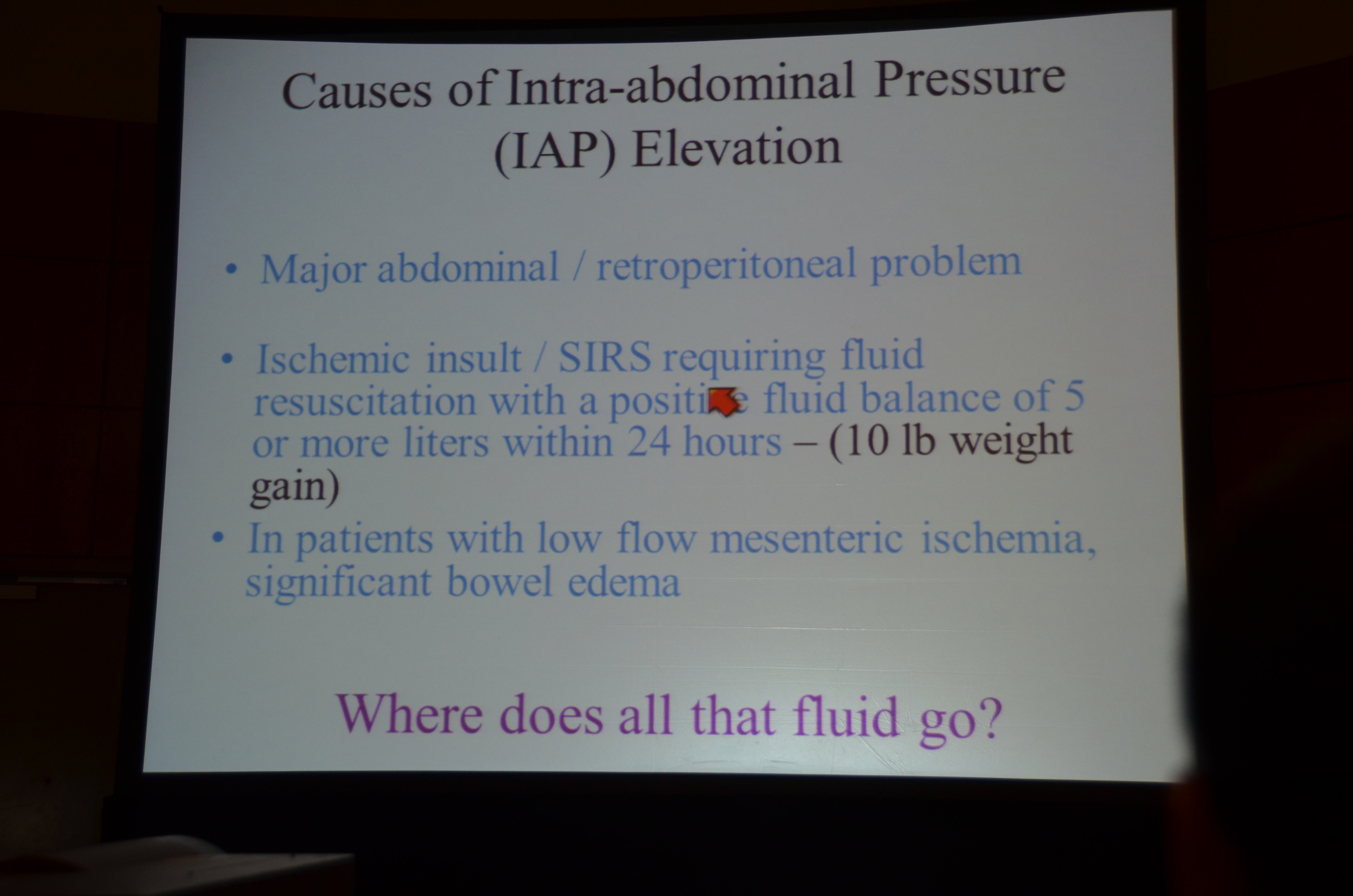
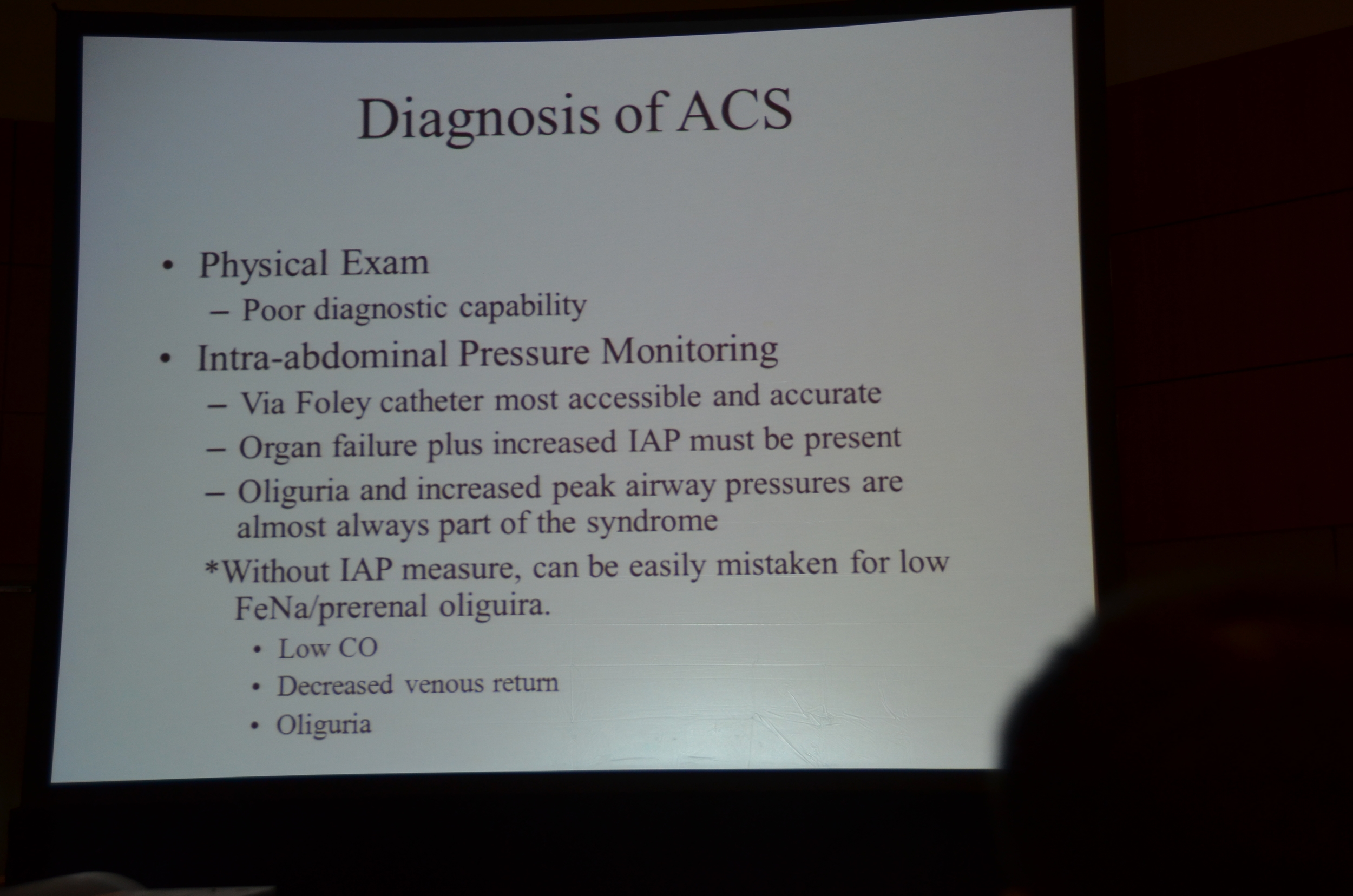
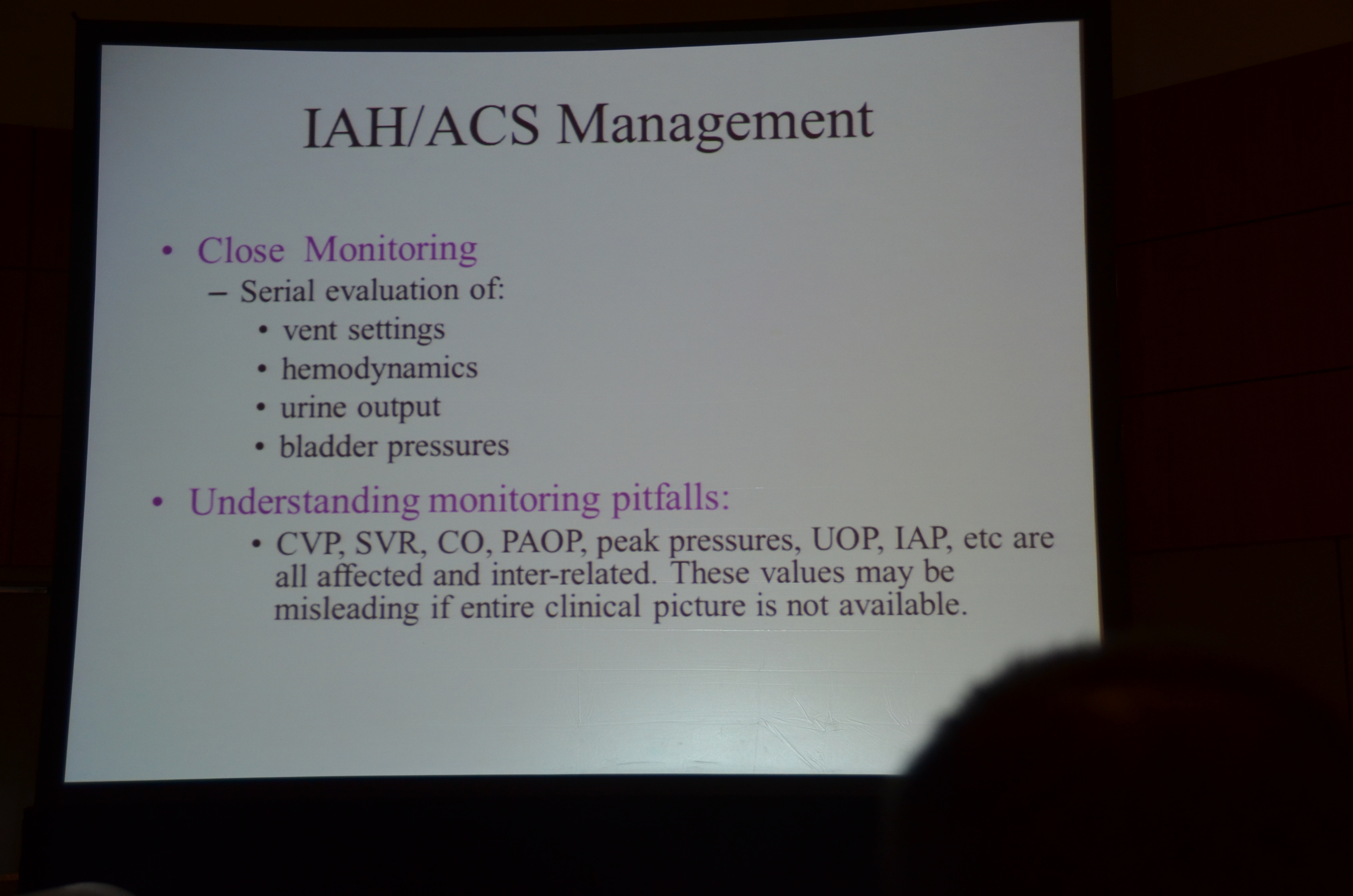
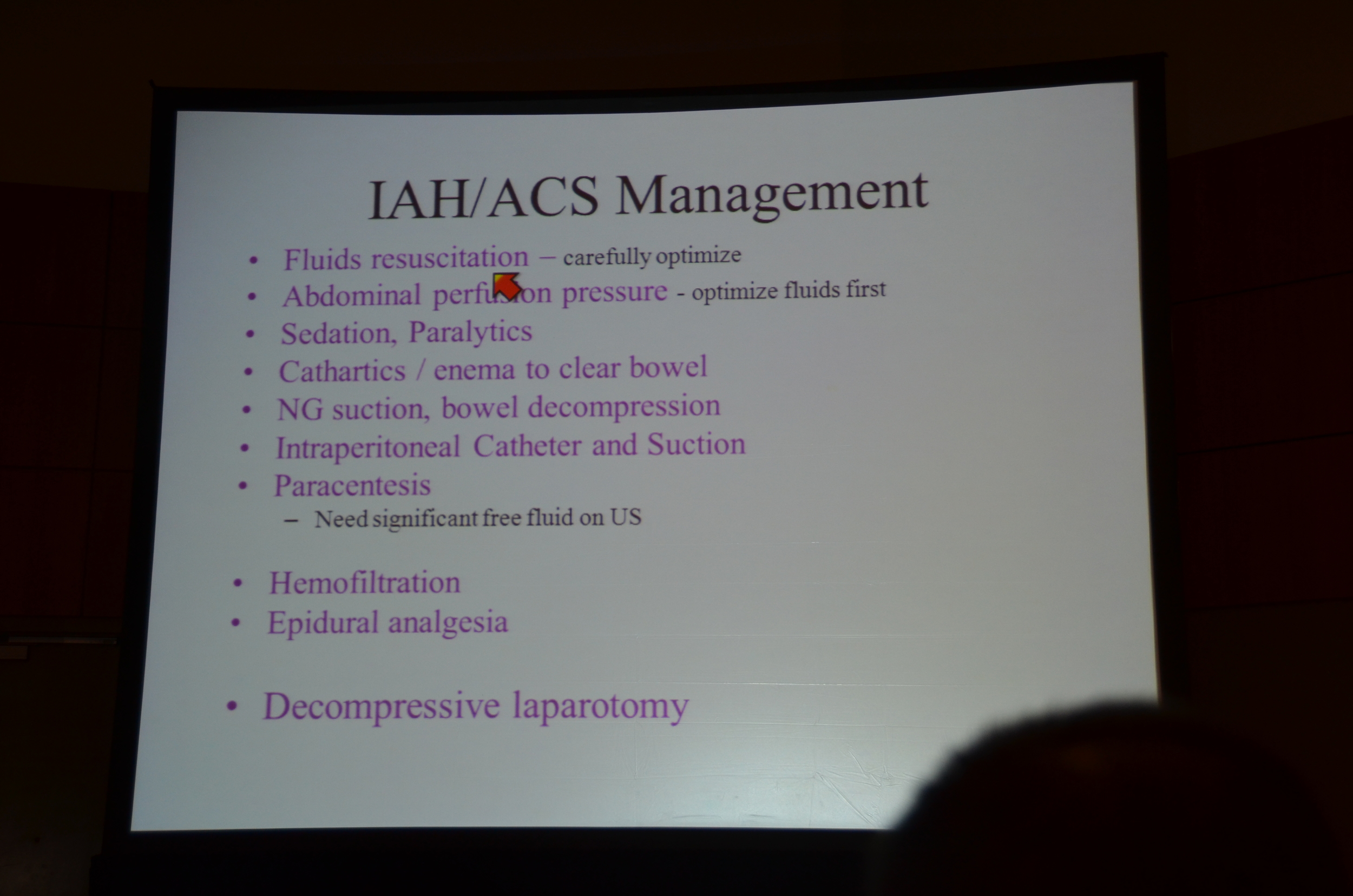
Abdominal Compartment Syndrome is defined as intra-abdominal pressure >12 mm Hg with organ failure, or an intra-abdominal pressure over 25mm Hg. Intra-abdominal hypertension can develop from:
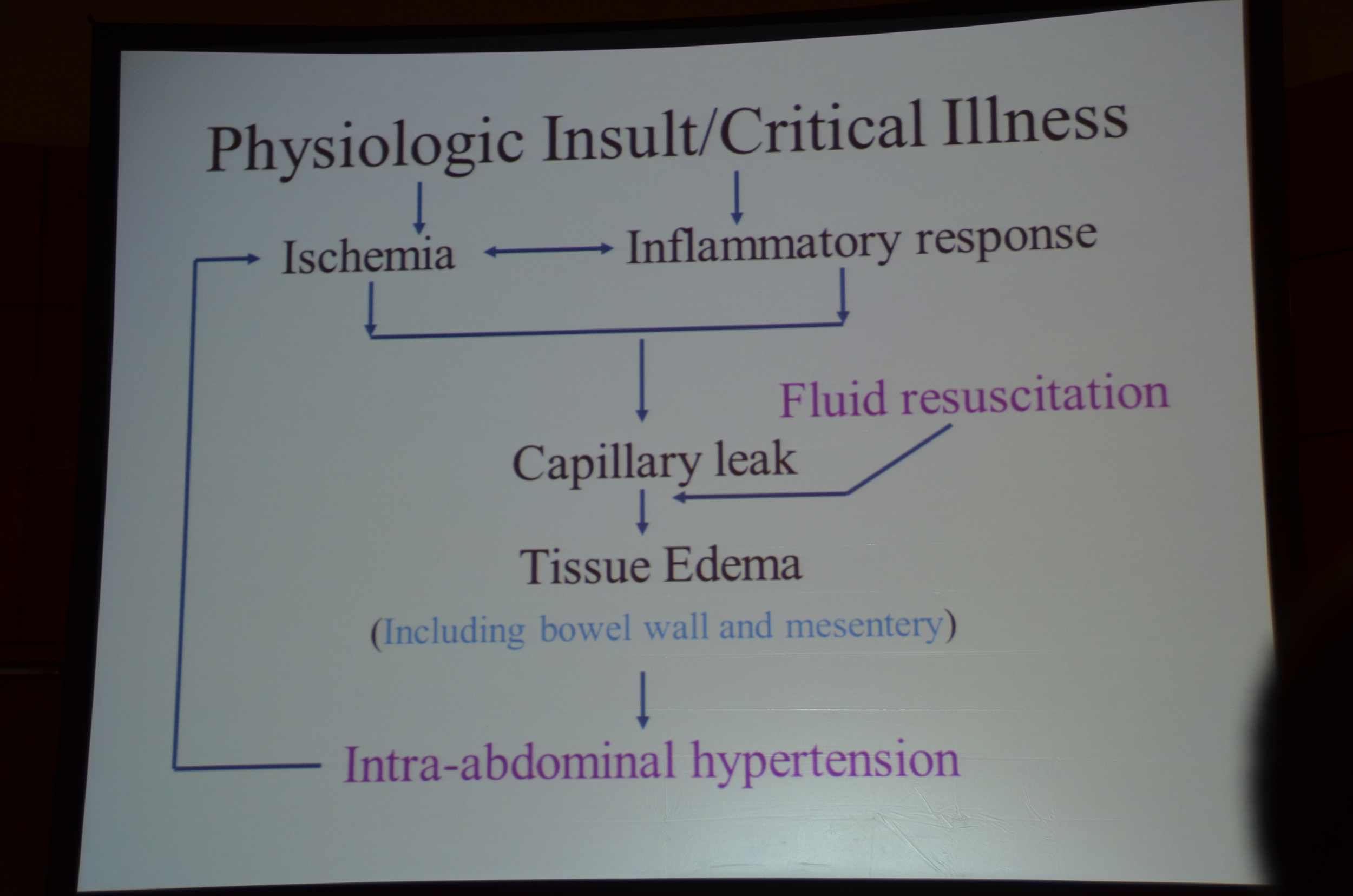
- Capillary leak from inflammation or ischemia, or
- Aggressive fluid resuscitation causing tissue edema.
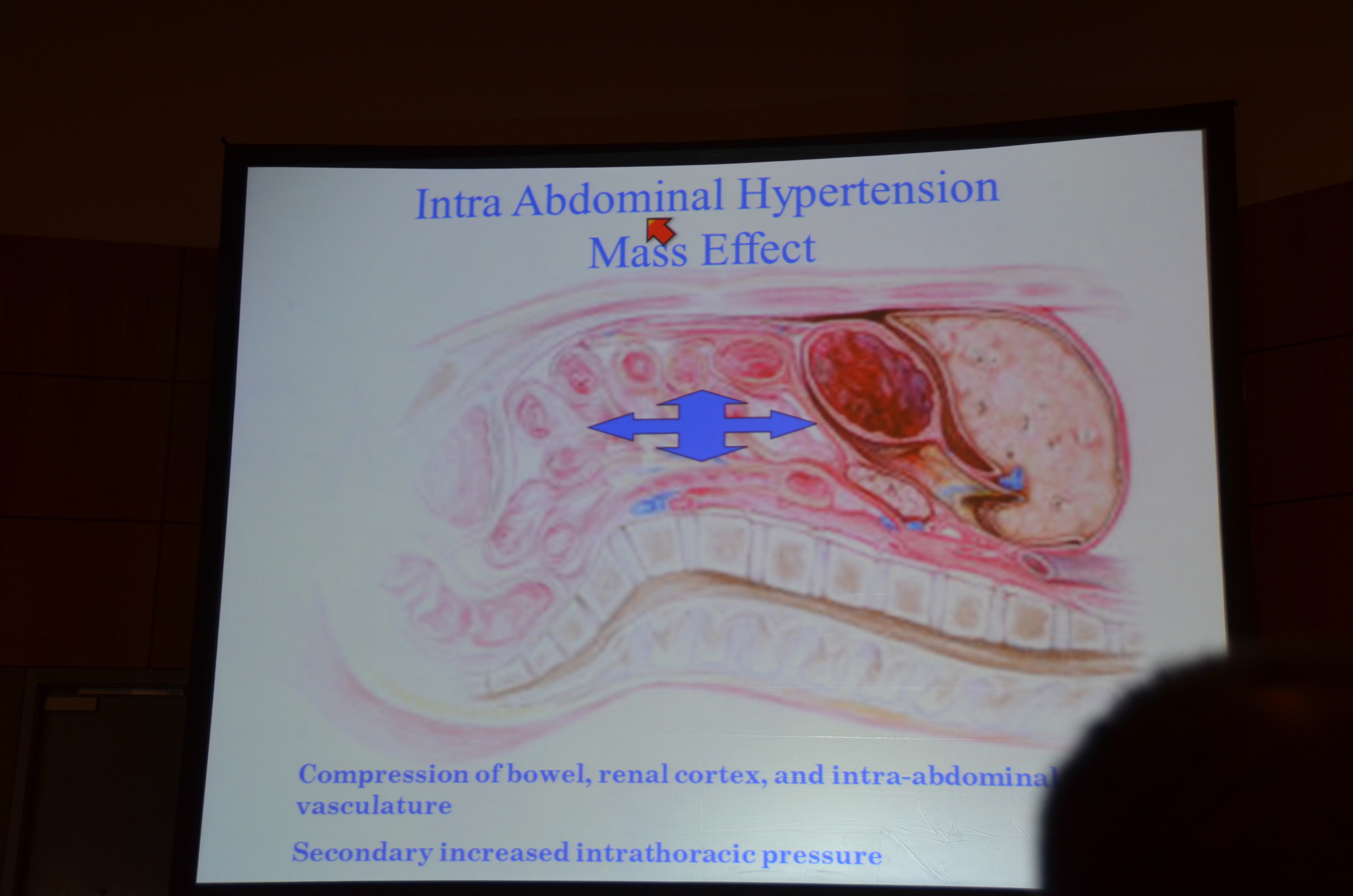
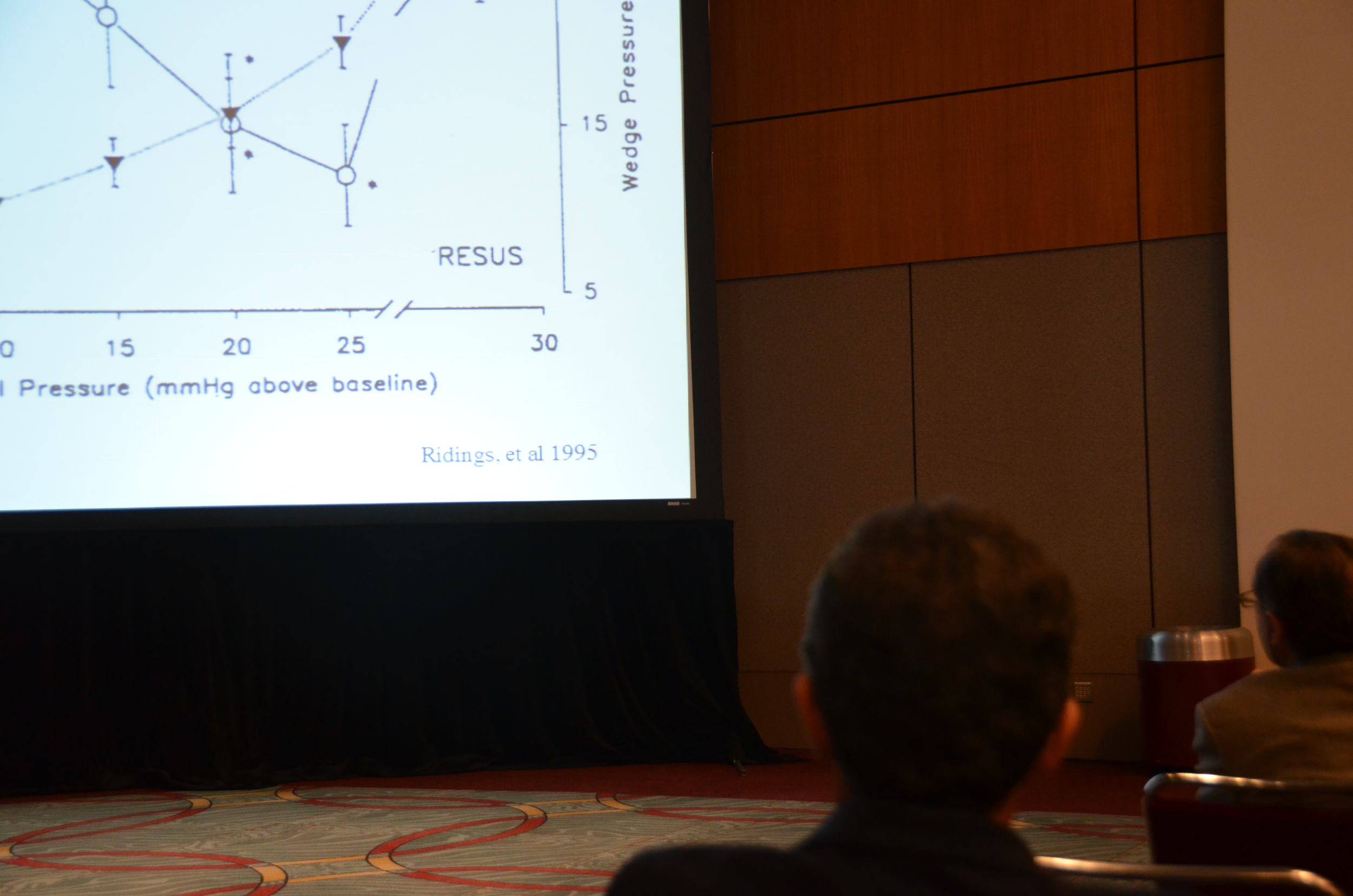
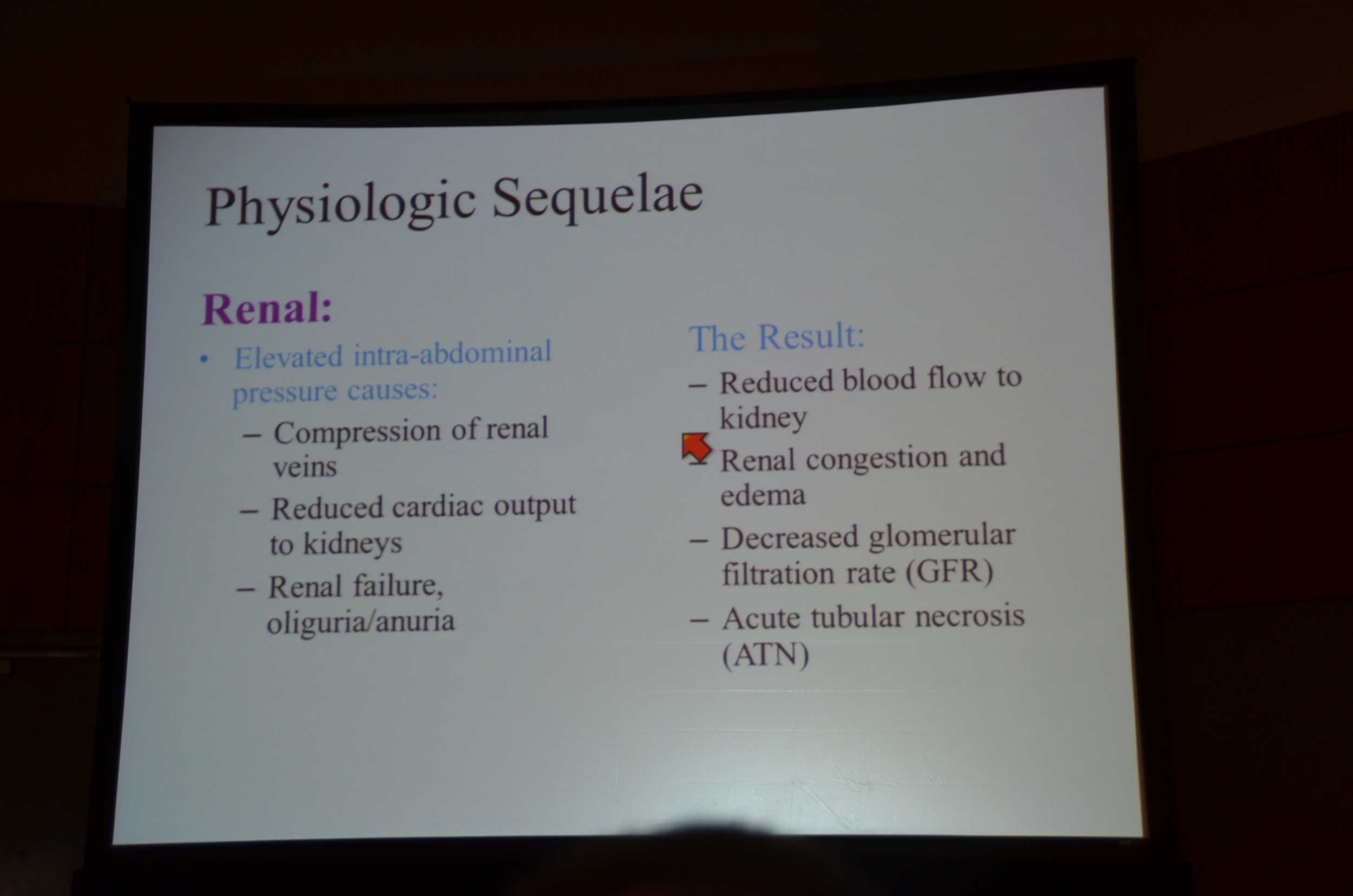
Intra-abdominal volume rises gradually because the abdomen is distendable but ultimately reaches a critical volume where the abdomen is maximally distended and then the pressure spikes. This increased pressure results in reduced blood flow and kidney injury.
Look for intra-abdominal compartment syndrome in patients with abdominal or retroperitoneal disease, resuscitation with more than 5 liters in 24 hours (10 pound weight gain) and in patients with low-flow mesenteric ischemia and bowel edema.
An interesting study was shared during this session:
To simulate the consequences of increased intra-abdominal pressure an experimental model was created by placing a 15 liter bag of water on the abdomen. Citerio et al found increased intracranial pressure, internal jugular pressure and increased central venous pressure.
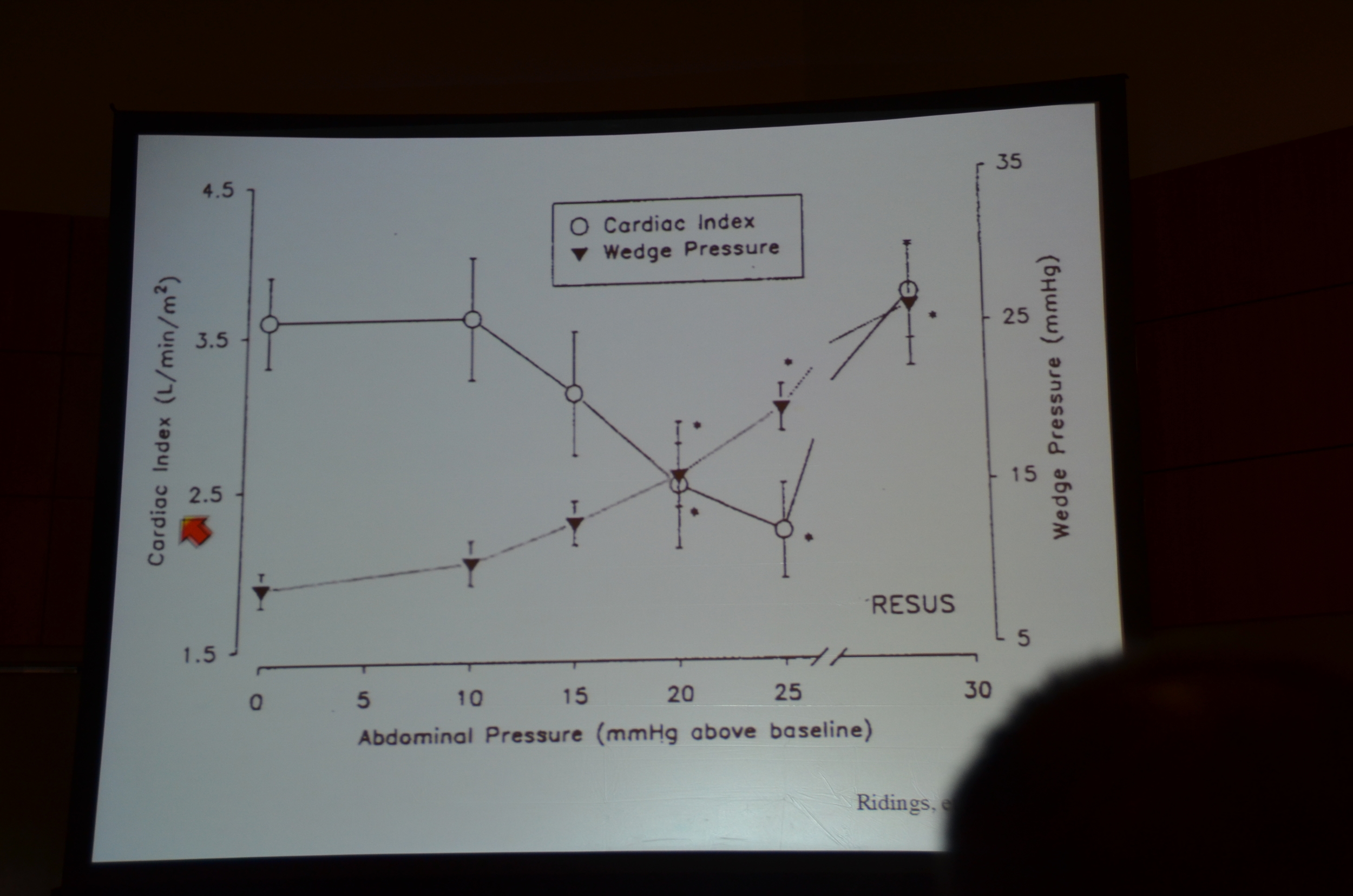
It also may increase the wedge pressure while dropping the cardiac index. Doctors may misdiagnose these indices as an adequate fluid resuscitation with primary cardiac dysfunction.
Renal sequelae include: reduced renal blood flow, decreased GFR, and ATN. The urinary indices look pre-renal, low FENa, oliguria.
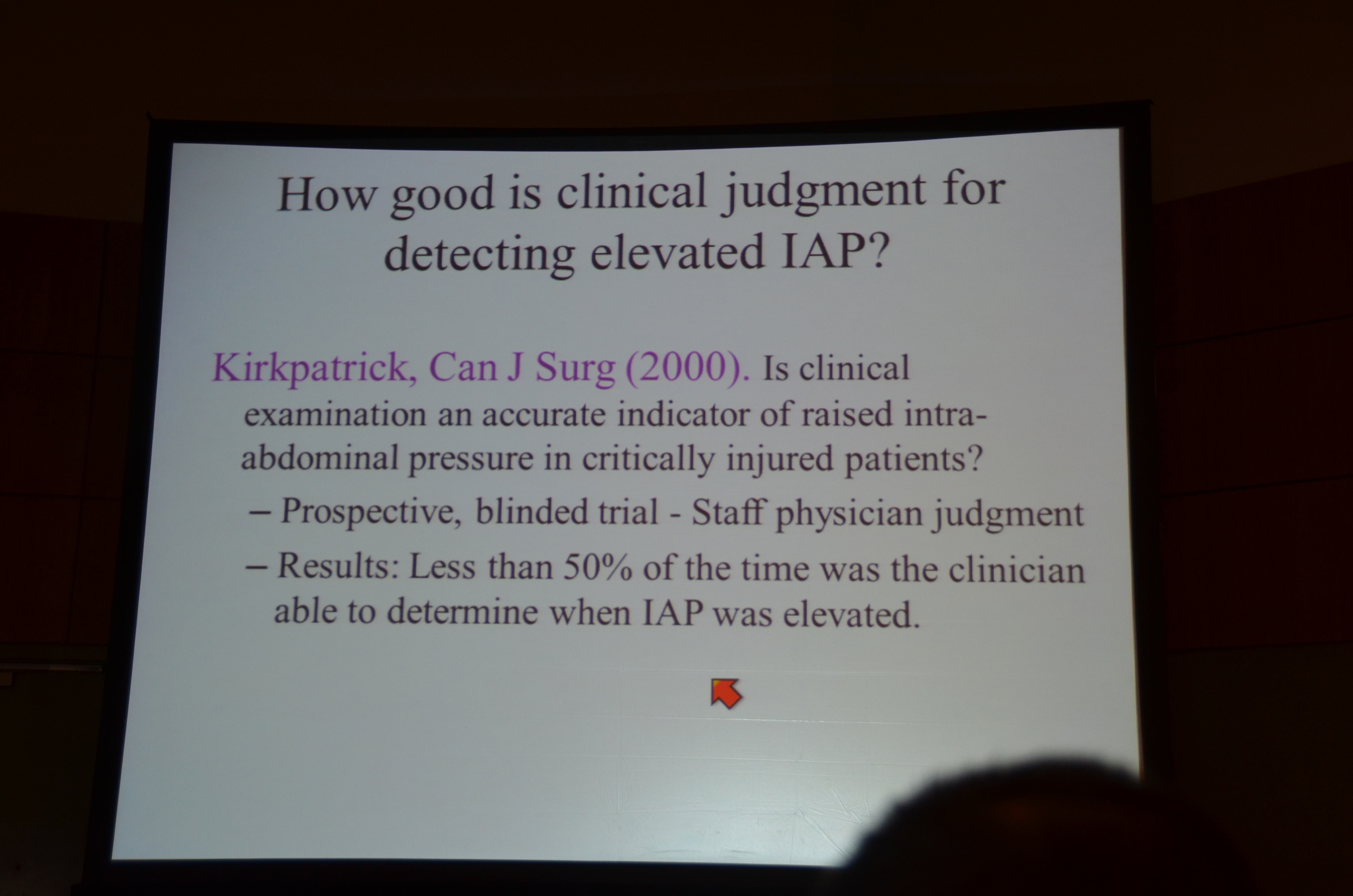
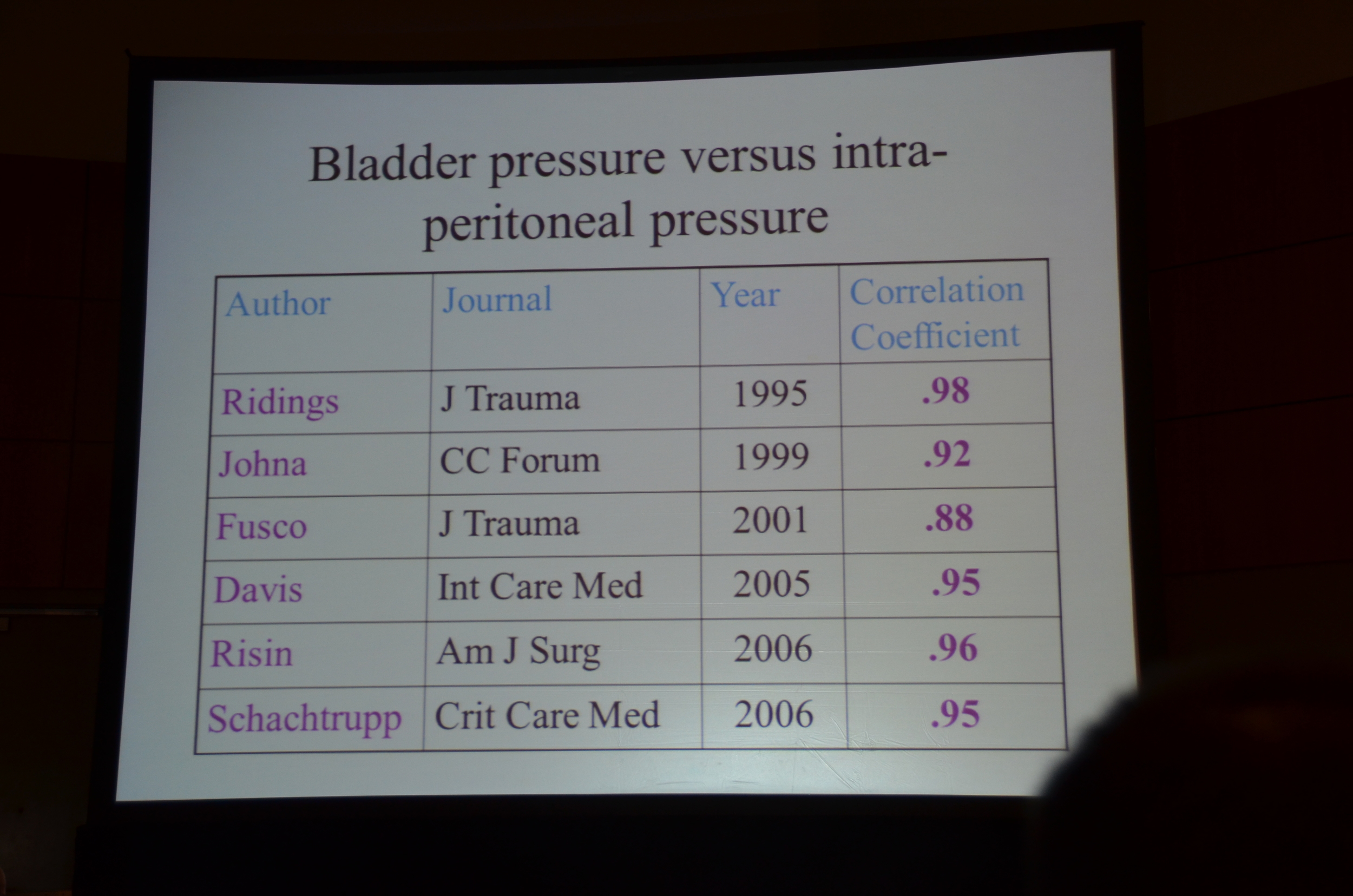
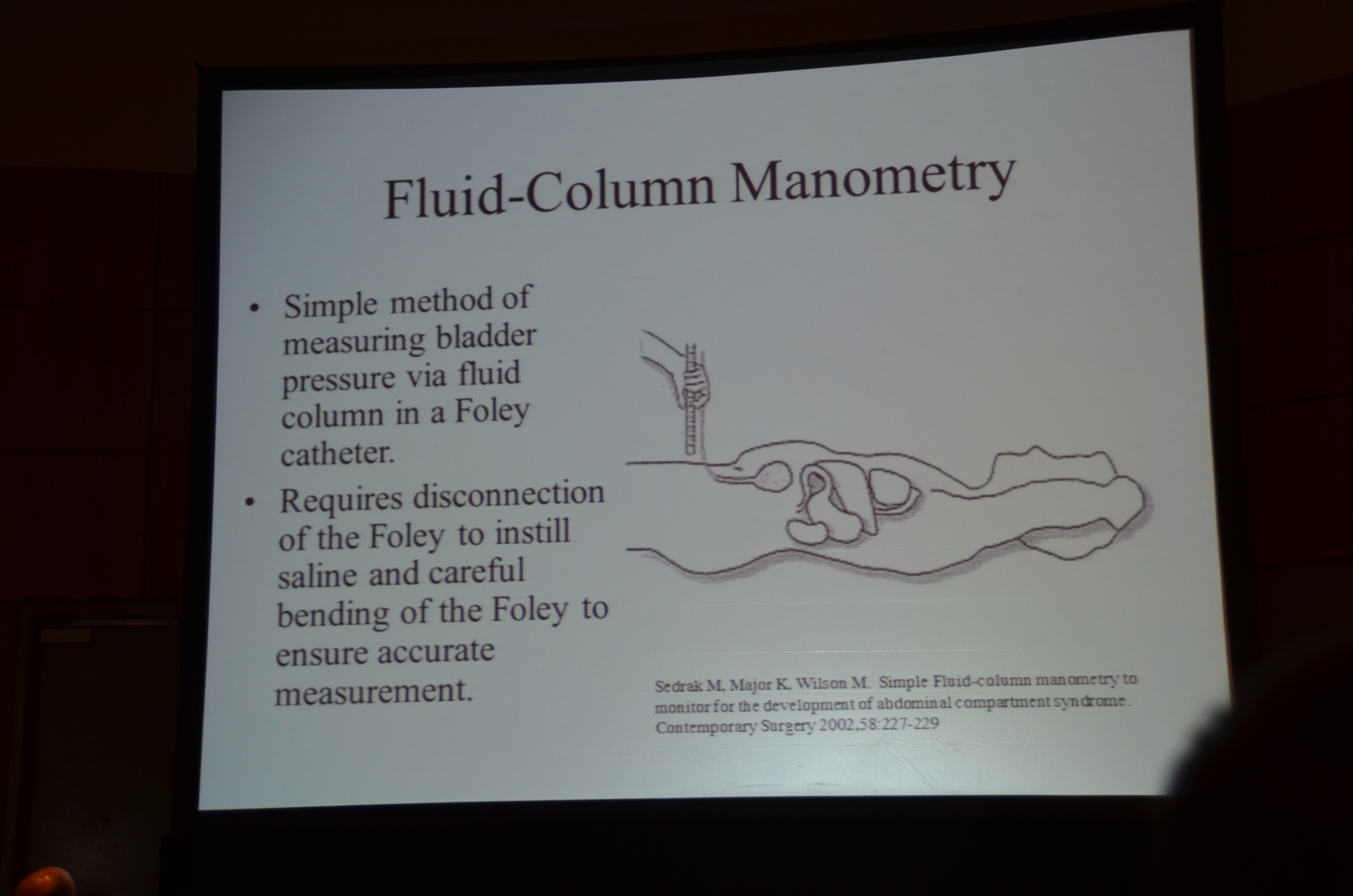
Physical exam is no better than a coin flip. Bladder pressure monitoring is needed.
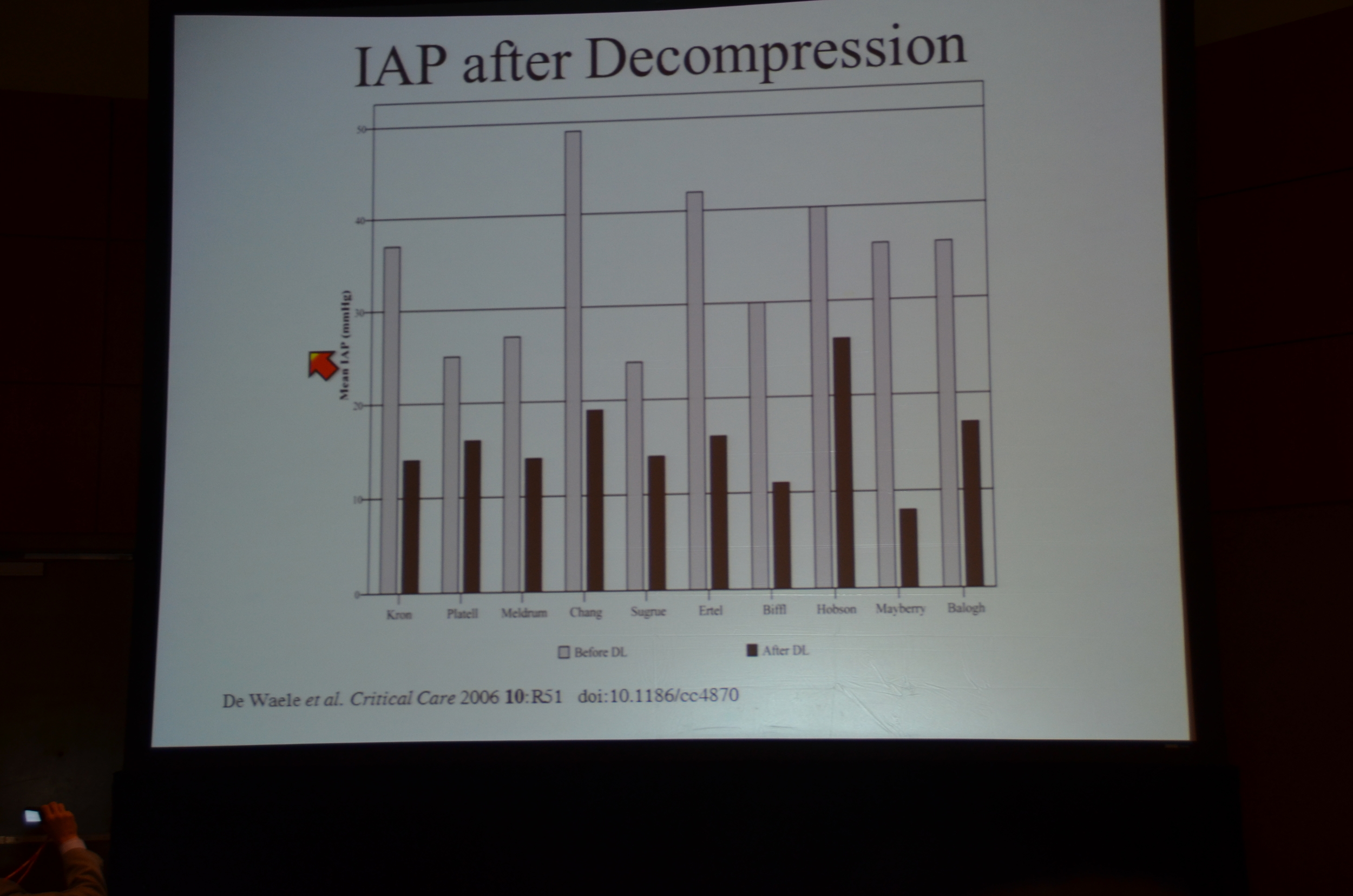
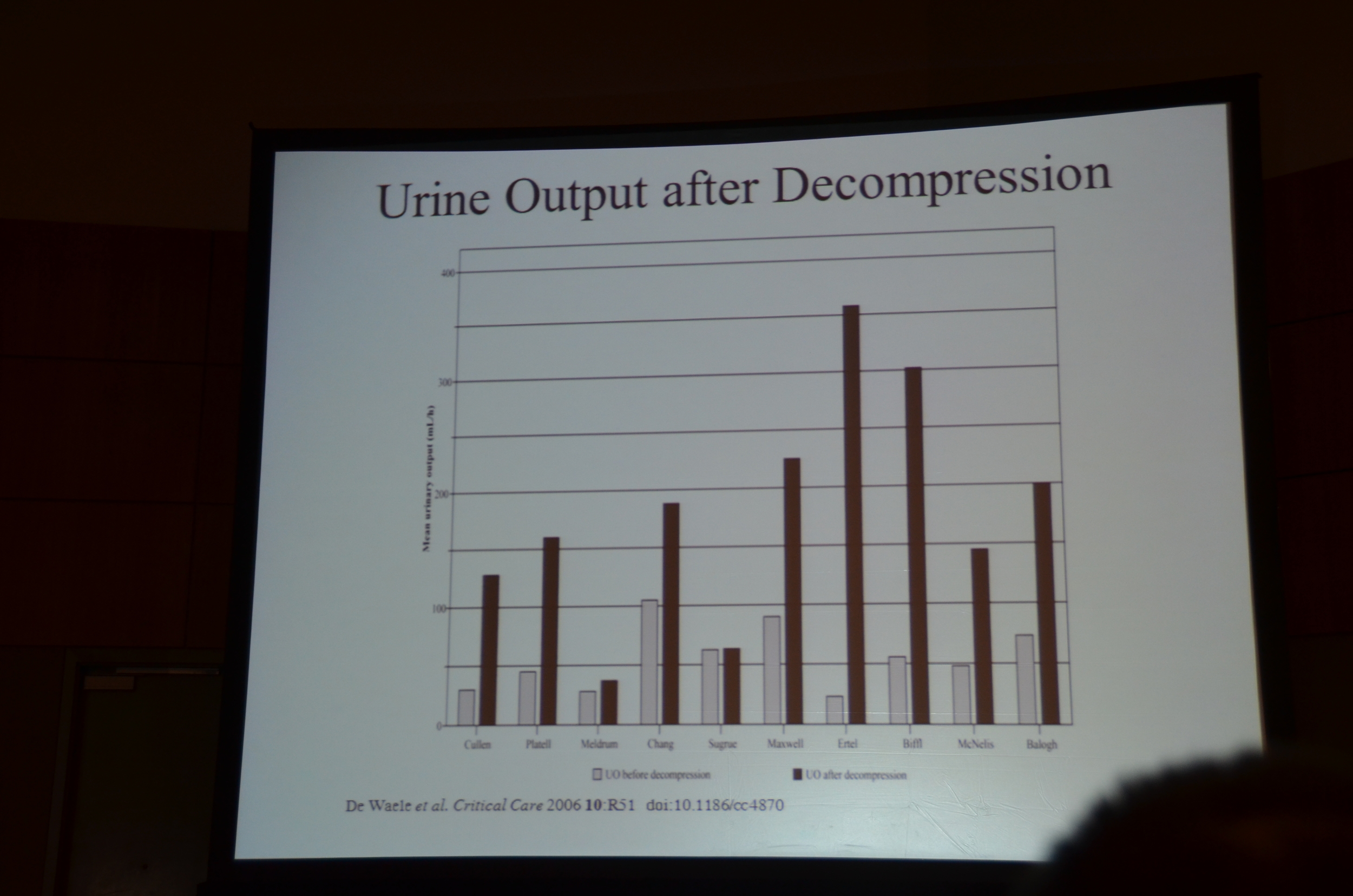
Dr. Chawla outlined a number of different treatment strategies including: optimize fluids, sedation, cathartics and enemas, NG suction, paracentesis and dialysis but ultimately noted that the definitive therapy is decompressive laparotomy. Delaying this may result in intestinal ischemia. Data from De Waele et al shows clear and consistent reductions in intra-abdominal pressure with laparotomy.
Conclusion: Intra-abdominal compartment syndrome is missed in the ICU because it is not considered in the differential for acute kidney injury and the cardiac indices point away from the abdomen and to the heart.
Remember the belly, save the kidneys.
My Live Tweet stream
Chawla up for AKI in the the Trauma Ward #KidneyWeek12
Trauma leading cause of death age 1-44
AKI in 0.32%, Mortality for all trauma was 2.5% #KidneyWeek12
That 0.32% was dialysis requiring AKI. #KidneyWeek12
0.32% of 2.5 million is 8,000, compare to 150,000 cases due to sepsis and 2,500 post cardiac surgery. #KidneyWeek12
Multiple studies find that AKI is independently associated with death. Like it is in every other disease. #KidneyWeek12
Huge typo on one of his slides, wrote 800,000, meant 8000. #fail #KidneyWeek12
Poor resuscitation increases risk of AKI. No reference. #Fail. #KidneyWeek12
CPK may not go up until late. Myoglobin goes up earlier. Again no reference. #KidneyWeek12
Intrabdominal compartment syndrome is increased pressure (>25 mmHg) and organ failure #KidneyWeek12
AWESOME picture of huge bowel edema with sausage like intestines squeezing through the bowel wall! Pic to follow. #KidneyWeek12
Causes effacement of IVC and renal veins on CT scan, but this should not be a radiologic diagnosis. #KidneyWeek12
Causes increased wedge and ICP and CVP. May be misdiagnosed as adequate resuscitation. #KidneyWeek12
Increased peak airway pressure, decreased ventilatory volume due to diaphragm being pushed north. #KidneyWeek12
Physical exam is not useless, but about as good as a coin flip. #KidneyWeek12
Use the bladder pressure! Very reliable. #KidneyWeek12
Treatment mainstay is decompressive laparotomy. Will need to leave the patient open for a few days. #KidneyWeek12
De Waele Crit Care in 2006 reviews the effectiveness of laparotomy. UO improves before your eyes! #KidneyWeek12
Trauma lecture is done. #KidneyWeek12
